Don’t follow the old pandemic trend anymore. In 2026, telehealth CPT codes have undergone an important transformation. It affects your medical billing, compliance and reimbursement across providers, practices and billing team. If you’re a healthcare provider, you need to know the updates, including new telehealth CPT codes.
This Guide breaks down everything you need to know, from new codes that change in 2025 to specialty-specific rules, with practical tips you can apply today.
Telehealth is a digital technology to allows healthcare providers to deliver care to patients remotely. Telehealth CPT codes 2025 are standardized numeric identifiers from the American Medical Association CPT code set that describe virtual healthcare services, like consulting via video, phone calls or brief virtual check-ins.
Why are they important:
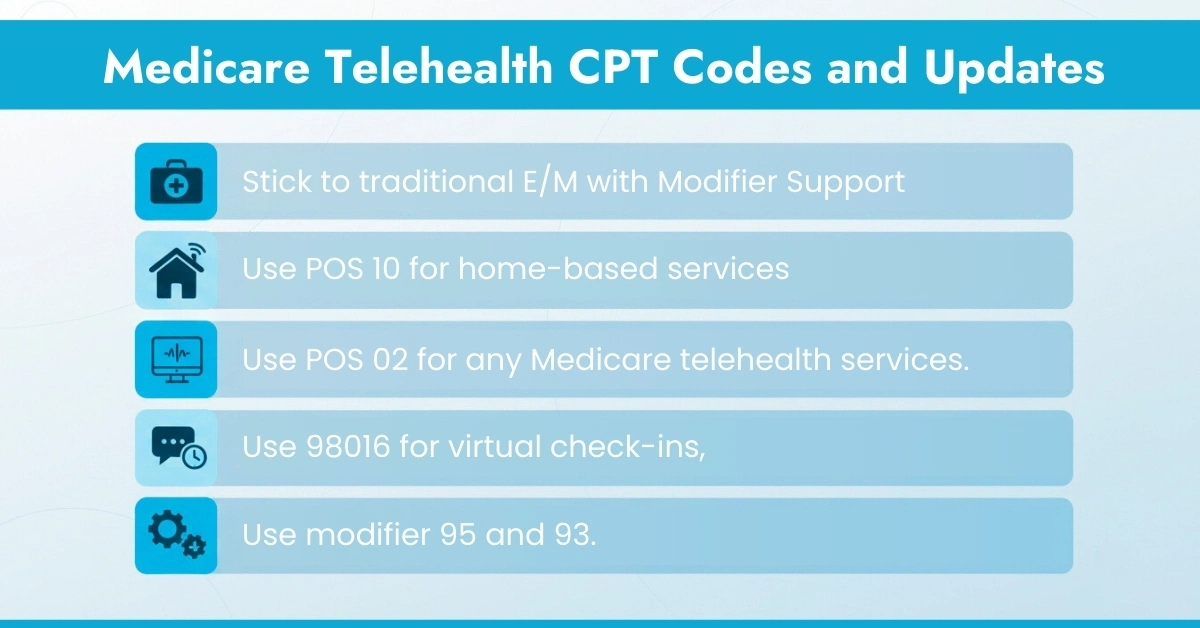
Before 2026, many telehealth services were billed using standard Evaluation & Management (E/M) codes, like CPT 99202 99215, along with modifiers 95 for interactive audio/video or 93 for audio-only, according to the Society for Maternal. Fetal Medicine.
The American Medical Association (AMA) introduced 17 new telemedicine-specific codes and deleting the old telephone evaluation codes.
Key additions are given below:
Code Range | Type | New or Est. Patients | Replaces | Purpose |
98000-98007 | Audio-Video | New and Established | Traditional E/M via telehealth | Real-time video visits |
98008-98015 | Audio-Only | New and Established | 99441-99443 | Medical discussion by phone |
98016 | Brief Communication | Both | G2012 | Short patient check-ins |
98016 is a new brief communication technology-based code that replaces the previous Medicare virtual check-in code G2012
Important:
These telehealth CPT codes are distinct from traditional E/M codes (99202-99215) and should not be reported together for the same encounter. The CPT telehealth codes update also clarifies that time-based billing requires explicit documentation of the total time spent on the date of service.
At HelloMDs, our medical coding services team reviews every encounter to ensure modifier and POS alignment, reducing rejections before claims leave your practice.
The American Academy of Family Physicians and CMS emphasize that Medicare allows audio-only technology only when the provider is technically capable of using audio-video, but the patient lacks the capability or doesn’t consent to video use. Your documentation needs to clearly state both conditions.
Audio-Only Billing Essentials:
Billing Tip: Some payers may still require traditional E/M codes (e.g., 99213) with a telehealth modifier when they haven’t adopted the new CPT codes. Always verify payer policies for compliance.
While we can’t cover every payer, let’s look at how Aetna telehealth CPT codes requirements might differ from Medicare:
Commercial payers like Aetna often:
Action step: Before each telehealth appointment, verify patient eligibility and benefits, ensuring telehealth coverage limits and any required authorizations are confirmed in advance. HelloMDs provides verification and denial management support to ensure accurate reimbursement regardless of payer policy.
Behavioral health leads telehealth adoption, and psychiatry telehealth CPT codes have specific rules:
These codes below are according to the Medicare Coverage Database (MCD)
Telehealth CPT codes bring clarity and structure to virtual care billing, separating audio-video, audio-only, and brief communication services. Medicare continues using traditional E/M codes with specific modifiers, while commercial payers may adopt new AMA codes. Accurate documentation, including time, medical decision-making, patient location, and technology used, is essential to ensure compliance and avoid claim denials. Specialty-specific codes, like psychiatry, require additional attention. Understanding these updates helps practices streamline telehealth workflows, improve reimbursement, and stay audit-ready.
Disclaimer
This content is for general information only and is not official medical or billing advice. Always confirm codes and guidelines with Hello MDs’ professionals. Some examples may be illustrative.
No. Commercial payers may adopt them at different times. Always check each insurer’s policy to determine which codes are accepted for reimbursement.
These older audio-only codes were deleted in 2025. AMA introduced 98008-98015 for audio-only visits, but Medicare still uses traditional E/M codes with modifier 93.
Yes, but document clearly for each service type. Use appropriate CPT codes, modifiers, and POS, ensuring compliance with payer rules for same-day billing.
Yes, psychiatry and behavioral health have specific CPT codes like 90791, 90834, 90837 for virtual evaluations and psychotherapy sessions, following payer and Medicare guidance.