If you are running a medical practice in Alabama, you face complex challenges, from managing state-specific requirements to complex insurance claims. Our AAPC-certified medical billing experts in Alabama know:
Partnering with Hello MDs’ billing experts ensures compliance, faster payments, and minimal claim rework.
Schedule a consultation
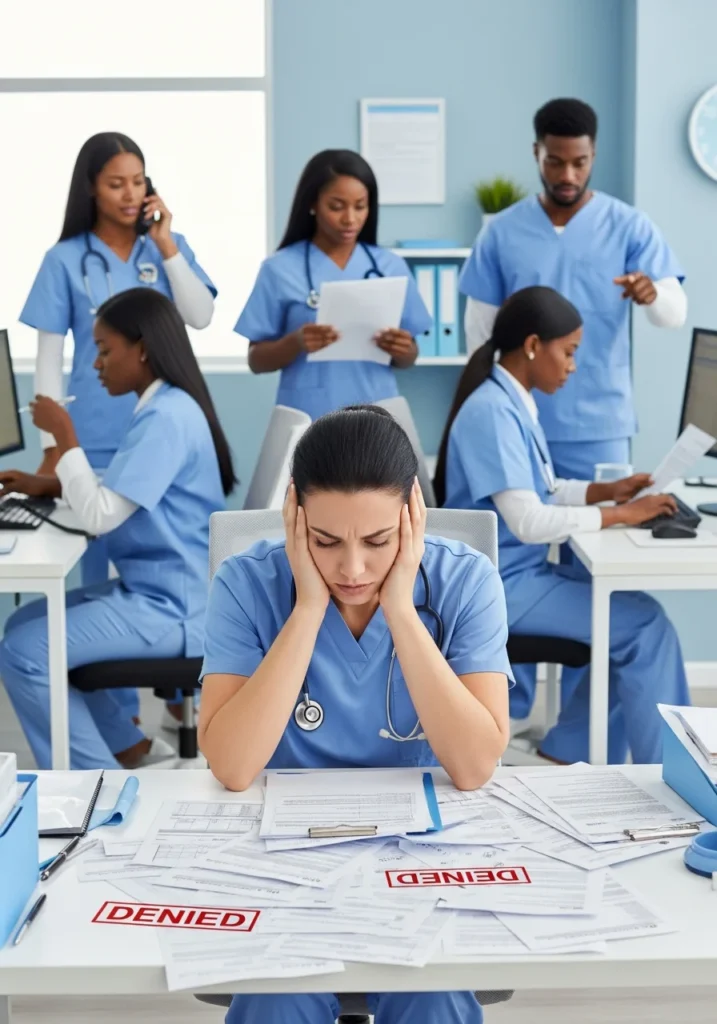
Many healthcare practices in Alabama lose thousands of dollars in revenue each year because of billing errors, including ICD codes like M54.9 and R10.9. Denied claims pile up, payment cycles stretch for months, and administrative costs drain resources that should go toward patient care. Manual coding mistakes, incomplete documentation, and missed filing deadlines create a cycle of financial stress that impacts your entire operation.
Hello MDs mitigate:
We make sure approvals happen on time so treatments and billing aren’t delayed.
We prepare and submit claims carefully, making sure charges and codes are entered accurately.
We record payments and adjustments correctly, giving you a clear picture of your incoming revenue.
When claims are rejected, we review the issue, follow up, and manage appeals step by step.
We verify coverage in advance to help prevent avoidable claim rejections.
We support each stage of the billing process, from registration through final payment.
HelloMDs provides medical billing company services to practices in these Alabama communities











We check your current billing process, identify revenue gaps, and create a plan to improve accuracy and efficiency.
Before each visit, we confirm insurance coverage and eligibility to ensure any required authorisations to reduce claim rejections.
Our certified coders carefully review documentation and assign proper codes to ensure correct billing.
Each claim is checked for completeness and submitted promptly to maximize timely reimbursement.

Payments are recorded accurately, underpayments are addressed, and summaries are provided to track collections.
We monitor outstanding claims, follow up with payers, and submit appeals with documentation to recover delayed payments.

Cleaner claims and faster reimbursements help practices increase income within months.

Access expert medical billing services in Alabama without extra staffing or overhead expenses.

Staff can focus on patient care and scheduling instead of handling billing tasks.

Accurate coding and billing management practices reduce rejected claims by up to 95%.

HIPAA-compliant processes and regular audits keep your practice aligned with all regulations.

Consistent payment posting and proactive accounts receivable management provide predictable monthly revenue.
Alabama practices choose HelloMDs for dependable, detail-focused medical billing experts support:
We have trained professionals who stay current with coding and billing requirements.
Our medical billers understand Alabama payer rules and reimbursement expectations, helping you avoid common billing issues.
We provide straightforward summaries so you can easily track claims, payments, and outstanding balances.
We onboard carefully, working with your existing workflows to avoid interruptions.
You work with a consistent team that understands your billing needs and day-to-day priorities.
We focus on cleaner claims, fewer denials, and more predictable cash flow over time.
Switching to HelloMDs was the best decision for our Montgomery practice. Our collections increased 28% in four months, and we finally have clear visibility into our revenue cycle. Their team responds immediately when we have questions.
Stop losing money to denied claims and slow payments. HelloMDs delivers trusted medical billing and coding services in Alabama to help you increase collections and reduce administrative burden.
Local medical billing companies understand Alabama payer rules, Medicaid variations, and regional reimbursement patterns, which helps reduce delays and avoid state-specific billing issues.
Medical billing experts typically hold AAPC certifications, complete ongoing education, and have hands-on experience with coding guidelines, payer rules, and compliance requirements.
Mobile medical billing allows billing tasks to be managed remotely while maintaining secure access, regular claim follow-ups, and consistent reporting without requiring on-site staffing.
Experienced billing teams monitor regulatory updates and adjust billing processes promptly to maintain compliance and prevent disruptions in claim submissions and reimbursements.
Warning signs include increasing denials, delayed payments, unclear reporting, rising receivables, and limited communication about unresolved billing issues.
Missing provider signatures or incomplete clinical notes. Lack of medical necessity documentation supporting CPT and ICD-10 codes.