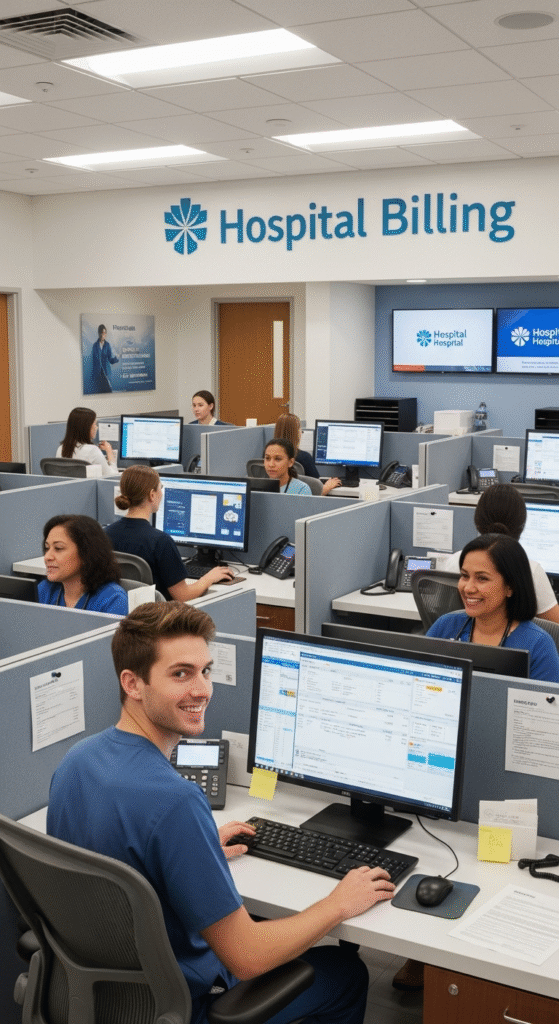
Struggling with delayed payments and billing errors? Our reliable hospital billing services ensure accurate claims, faster collections, and stress-free patient billing. We know your concern because we know that facts that billing mistakes drain $935M weekly, and annually it has reached about 125 billion from U.S. healthcare providers. Do not worry, every problem has multiple solutions in different shapes, but your only work is to find and grasp the opportunity.
Hello MDs, a trusted medical billing partner of the USA delivers accurate, compliant hospital billing solutions that reduce denials, speed up collections, and ease admin strain. Contact us today for a free consultation.
Schedule a consultation

Managing hospital finances can be challenging without efficient systems because many healthcare providers lose their revenue annually. Hello MDs’ services offer complete patient billing solutions along with hospital billing and collection services. This service helps hospitals to increase revenue, reduce errors, and ensure compliance day by day. As a trusted hospital billing company in the USA, we provide customised solutions tailored to your hospital’s size and speciality.

We manage complete hospital billing services, including claims processing, insurance verification, and payment posting. Our team ensures accurate billing and faster reimbursements.

Hello MDs’ patient billing solutions simplify invoicing, provide clear statements, and reduce patient queries related to insurance. Our service improves patient experience and speeds up collections. Our billing team gives you daily reporting.

We offer full customised hospital billing and collection services, from claim submission to follow-up on denials. Our approach ensures minimized delays and improved cash flow.

We handle specialty claims, coding, and reconciliation, ensuring doctors get paid accurately and on time. Our in-house team has proper knowledge of ICD codes like E11.9, I10 , M54.5 , J18.9 and N39.0 etc that are responsible for common denials.

If you are in Texas to Chicago, or other states of the USA, we always value your concern related to RCM services. HelloMDs are HIPAA compliant and provide services throughout the state of USA.
We are an experienced hospital billing company in the USA, backed by 100+ in-house team members who have been servicing for years, delivering accurate and timely revenue solutions.
Comprehensive and customize patient billing solutions to reduce errors and improve patient satisfaction.
Advanced hospital billing systems integrated with your existing workflows. We have expertise on how to streamline your billing costs effectively.
We are a professional physician billing service provider for hospitals and clinics to ensure timely reimbursements with an almost 99 percent success rate.
Trusted medical billing service in the USA with proven results and compliance. We read your denials thoroughly and understand the reason behind it, and then reimburse it with your link insurance provider.
We provide full hospital billing and collection services. You do not pay extra for other services related to it. Moreover, we ensure to maximise revenue and streamline operations.
Your Recovery Starts Here, From the First Consultation to the Final Payment
Evaluate current billing systems and identify revenue leakage or inefficiencies in your hospital billing and patient services.
Develop a tailored hospital billing solution with the help of medical billing team for improved accuracy and faster collections.
Implement modern hospital billing systems and software that integrate seamlessly with EMRs.
We identify coverage gaps, incorrect patient data, and coding mismatches using EMR-integrated denial analytics before they stall your revenue recovery cycle.
Provide clear patient billing solutions, statements, and support to enhance patient satisfaction.
Monitor metrics, track revenue, and continuously improve billing efficiency.
Reduces errors and claim denials upto 99 percent with us.
Optimizes cash flow with efficient hospital billing support.
Offer transparent patient billing solutions to enhance trust, just like 120 companies trust us.
We regularly read the updates and follow strict healthcare billing regulations of Centers for Medicare & Medicaid Services, OIG, OIR, etc.
We streamlined operations with modern hospital billing systems. We do not follow the old rules that cause denials
You can reduce administrative overhead and operational costs by outsourcing our services.
HelloMDs streamlined our hospital billing overnight. Our team stopped chasing denials—it’s all tracked. Cash flow improved within weeks. Integration with Cerner works. Highly recommend.
Stop losing revenue to billing inefficiencies. Partner with us, a trusted hospital billing company that delivers accurate, reliable, and compliant hospital billing services. Contact us today for a free consultation and maximise your hospital revenue!
We file all claims electronically, track each one for status, and consistently follow up on denied or rejected claims to maximize successful resubmission.
We keep it transparent, pricing scales with your hospital size and service needs. You only pay for results, no hidden fees or surprise charges.
Yes. We use encrypted data storage, conduct regular security audits, train staff continually, and strictly limit PHI access to authorized personnel only.
We offer 24/7 support. Hospital administrators reach a live RCM specialist quickly—no voicemail queues, no delays in addressing critical billing questions.
Absolutely. We support telehealth CPT codes (e.g., 99443) and ensure reimbursement for Medicare, Medicaid, and private payers, adjusting for state-specific guidance.
Attending physicians can bill for discharge services. Hospitals bill separately for facility-related fees. We manage each stream to prevent duplicate or denied claims.
Yes, if appeals are successful. We handle the entire denial appeal process to secure coverage before any patient billing is issued.