Hello MDs medical billing company helps Independent Physician Associations (IPAs) recover lost revenue and maximize reimbursements for your 2025-26 denials. With 99% accurate claims powered by Robotic Process Automation (RPA), we ensure faster insurance payments and full compliance with new Florida’s medical billing laws and guidelines. Our achievements have catched attention of healthcare providers of FL through;
HelloMDs delivers HIPAA-compliant medical billing solutions across Florida, offering end-to-end revenue cycle management services that place it among the leading medical billing companies in Florida.
Schedule a consultation

Our medical biller knows that Florida medical practices face increasing administrative and financial pressures in today’s healthcare landscape. Moreover, we are eyeing industry reports showing claim denials remain a key challenge. We are aware that many providers are experiencing denial rates between 15–20% due to documentation, coding, and eligibility issues. In 2026, Florida’s New Refund Law states that you must prepare for new state requirements that mandate refunding patient overpayments within 30 days beginning. HelloMDs removes these challenges with comprehensive Revenue Cycle Management (RCM) solutions for Florida practices.
What do we do?
Quickly handle insurance approvals to prevent delays and claim rejections.
Ensure accurate coding for clean claims and faster reimbursements.
Monitor unpaid claims and recover revenue to stabilize cash flow.
Enroll providers efficiently with insurance networks to keep billing uninterrupted.
Support for compliance and accreditation of medical equipment to meet Florida standards.
Reduce administrative workload with professional support for daily operations.
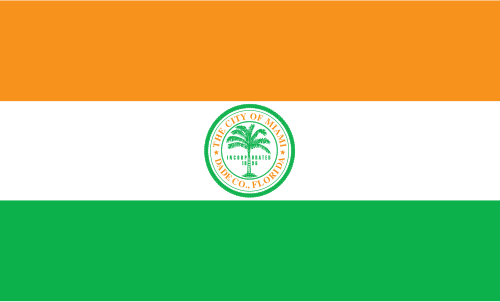
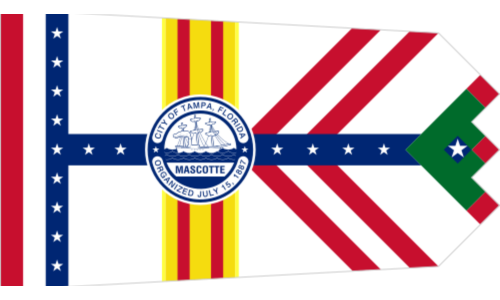
We provide billing services across the state, including major cities of Florida like:




Our in house experienced medical billing team has extensive experience working with Florida’s top payers, including AARP, Aetna, etc. We navigate payer-specific rules and policies to maximize reimbursements for your practice.
Pay only for the services you actually use, like denial management, payment posting or others. Our flexible pricing models are designed specifically for medical groups of all sizes, ensuring high-value billing solutions that fit your budget.
We prioritize compliance with HIPAA and Florida medical billing regulations and authorities. Our Nevada billing experts safeguard your practice from audits and penalties with proper medical billing audits.
Access real-time insights into your revenue cycle with detailed reporting and insights that make it easy to track your practice’s revenue and financial health.
We understand Florida’s payer rules and state reporting nuances, which helps to reduce claim rejections and improve your collections.

We review your current billing process to find missed revenue, compliance gaps, and areas to improve, according to Florida billing guidelines and laws.

Our team works with your existing systems without disrupting your daily operations, like patients etc. Otherwise we handle through previous data.

We handle accurate charge entry, apply correct CPT and ICD-10 coding per AMA guidelines and Florida payment schedules rules, and submit clean claims for faster approval.

Our specialists identify denial patterns in rejected claims, appeal them properly, and prevent future denials.

We do payment posting accurately, track reimbursement trends, and make sure every dollar reaches your practice.
We continuously monitor your revenue cycle performance, adjust to Florida regulations, and give tips to boost your financial performance over time.
Our proven approach to medical billing in Florida operations typically increases collection rates by reducing denials, accelerating payments, and recovering previously written-off accounts.
Stay compliant with HIPAA, Florida state regulations, and payer-specific requirements through our vigilant monitoring and expert knowledge of evolving healthcare laws.
Free your staff from time-consuming billing tasks, allowing them to focus on patient care, scheduling, and other activities that directly improve practice operations.
Experience quicker cash flow with our efficient claims processing, systematic follow-up on outstanding receivables, and proactive communication with Florida insurance companies.
Our accurate coding, thorough documentation review, and knowledge of payer requirements significantly reduce claim rejections and the costly rework they require.
Gain valuable visibility into your practice’s financial performance with comprehensive reporting that highlights trends, opportunities, and areas requiring attention for continued growth.
HelloMDs transformed our billing department completely. Within 60 days, our accounts receivable dropped by 45%, and we're finally collecting what we've earned. Their team knows Florida payers inside and out.
Stop losing money to claim denials, payment delays, and administrative inefficiency. Hello MDs provides certified medical billing services for small practices and large clinics across Florida and its affliated cities, delivering results you can measure from day one. Our AAPC-certified billing specialists handle all aspects of your revenue cycle with precision and care.
Florida has unique insurance rules, state regulations, and reporting requirements, so local billing services like Hello MDs ensure faster, compliant, accurate claim processing.
Most practices notice faster claim approvals, reduced denials, and improved cash flow within 30-60 days after partnering with HelloMDs.
Yes, we provide billing for about 48+ specialities, including primary care, cardiology, therapy, and more, tailored to each practice’s needs. See here.
We identify denial patterns, correct errors, appeal rejected claims, and implement strategies to prevent future denials efficiently.
Our team follows strict HIPAA policies, secure systems, and continuous staff training to protect patient information and maintain compliance.
Yes, we review past accounts receivable, submit appeals, and recover unpaid claims, helping practices improve cash flow quickly.