Home / Describe the PMS and How It interacts with the EHR
Your front desk schedules a patient in your practice management system. Your clinical team documents the visit in the Electronic Health Records (EHR), but when billing time arrives, someone manually re-enters diagnosis codes (ICD-10 M54.5 for low back pain), insurance details, and procedure notes, which introduces errors that cost you money. The duplicate data entry between the Practice Management System (PMS) in healthcare and the EHR software slows your revenue cycle and creates denied claims. This is why it is essential to describe the PMS and how it interacts with the EHR in a clear, practical way with professional help.
According to research from the American Academy of Professional Coders (AAPC), integration gaps between administrative and clinical systems contribute to nearly 20% of claim denials in medical practices.
A practice management system definition starts with its core purpose: managing the business side of healthcare. While your electronic health record’s meaning centers on clinical data, PMS for clinics handles administrative operations that keep your doors open.
Key PMS features in healthcare include:
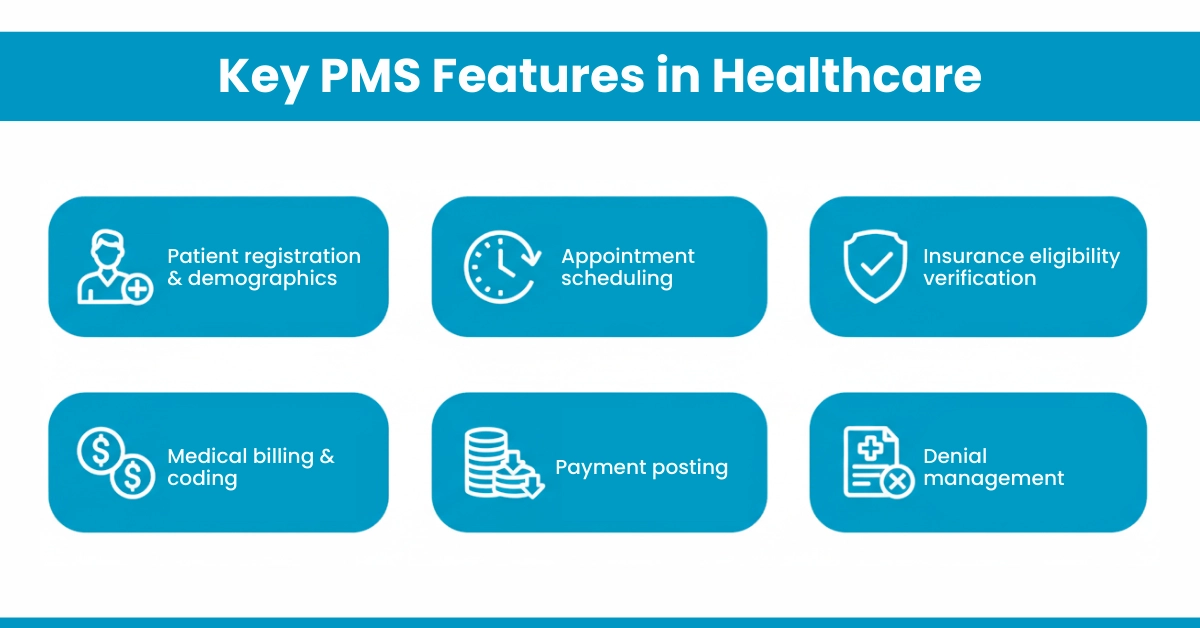
The PMS for clinics focuses exclusively on operational workflows. When your front desk schedules an appointment, verifies insurance coverage, or processes a payment, they’re working within the PMS environment. However, the PMS typically does not store clinical notes, treatment plans, or diagnostic information; that’s where the EHR comes in.
PMS play a critical role in coordinating billing workflows across different healthcare settings. To better understand how billing functions within a PMS-EHR ecosystem, explore Types of Medical Billing, which explains how integrated systems support accurate claims processing, reduce administrative errors, and improve revenue cycle efficiency.
An EHR definition focuses on the clinical lifecycle. EHR software creates, stores, and manages patients’ medical histories electronically, replacing paper charts.
The modern EHR benefits in healthcare are given below:
For your information: The CMS EHR toolkit emphasizes that clinical workflow software must capture structured data that supports quality reporting and population health initiatives. Your EHR contains the clinical evidence that justifies every billed service.
The differences between the primary functions of Electronic Health Records and Practice Management Systems are outlined below, providing a clear understanding.
Aspect | Practice Management System (PMS) | Electronic Health Record (EHR) |
Primary Focus | Business & Administrative Operations | Clinical Care & Patient Health Data |
Core User | Administrative Staff, Billers, Office Managers | Physicians, Nurses, Clinical Staff |
Key Functions | Scheduling, Billing, Insurance Verification, Reporting | Clinical Documentation, Order Entry, Decision Support |
Main Data Output | Financial Claims, Revenue Reports | Patient Health Records, Clinical Notes |
The PMS and EHR integration work together through a bidirectional data exchange that eliminates silos. Here’s exactly how PMS connects to EHR in daily operations:
The Core Exchange Flow
When PMS and EHR systems are not integrated, practices are forced to manually reenter data at multiple stages of care delivery and billing. This manual handoff is a major source of errors
Did you know? Medical billing audits frequently reveal that 15-20% of billing and claim errors originate from manual data entry caused by missing or poorly configured PMS and EHR integration.
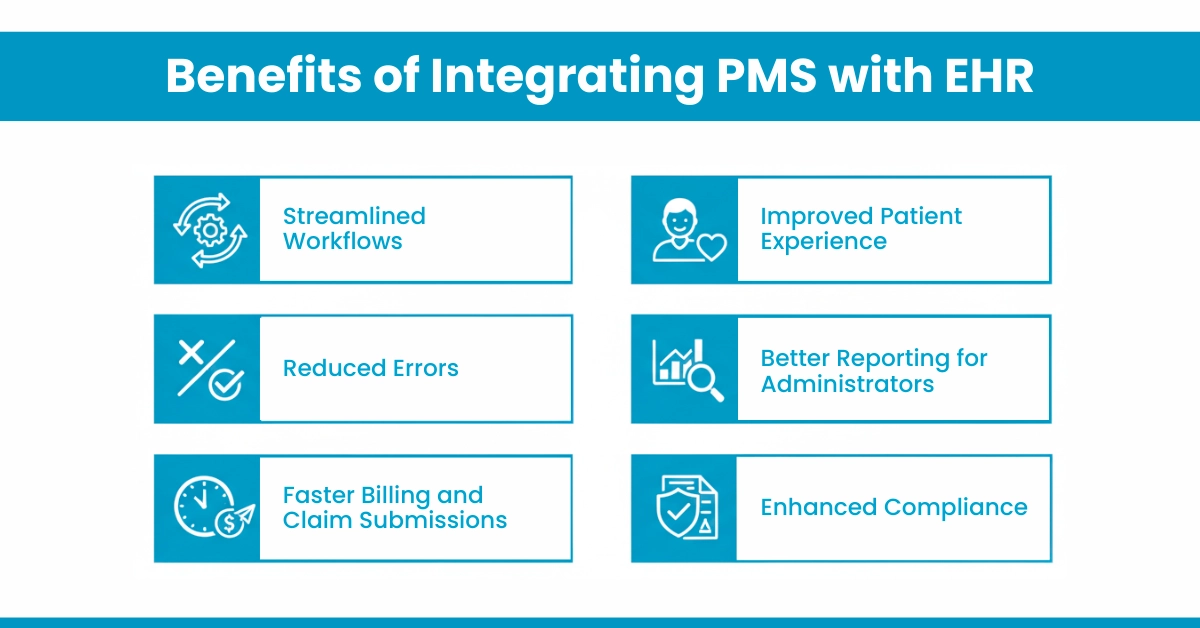
Integrated PMS and EHR systems solve multiple ICP pain points simultaneously. Here are the measurable advantages:
Advice from Hello MDs: Our denial management specialists find that integrated systems reduce claim denials by 25% because clinical documentation matches billed services precisely.
Follow these PMS and EHR implementation tips to maximize success:
For your information: Practices see ROI within 6-12 months through reduced denials
Here are some challenges that mainly occur in PMS-EHR integration:
A PMS handles your business; an EHR manages clinical care. When they interact seamlessly, you eliminate duplicate data entry, accelerate payment posting, and reduce denied claims tracking headaches. The result: healthier revenue cycles and happier patients.
Our AAPC-certified coders and billing specialists help practices achieve 95%+ first-pass claim acceptance by optimizing PMS and EHR workflow.
Whether you need prior authorization support, denial management, or full RCM healthcare services, we ensure your systems work together, not against each other.
Disclaimer:
For informational purposes only and not a substitute for professional medical or billing advice. Verify all codes and procedures with certified professionals. Some images in this article are AI-generated or used for illustration purposes only.
A PMS streamlines appointment booking, tracks patient visits, sends reminders, manages cancellations, and ensures efficient front-desk workflow.
Integration occurs via native APIs, middleware platforms, HL7 or FHIR standards, ensuring seamless data exchange between PMS and EHR.
Providers, billing teams, administrative staff, and patients benefit from reduced errors, faster billing, better scheduling, and improved care coordination.
Integration maintenance is shared between IT teams, software vendors, and practice administrators to ensure smooth, secure, and compliant operations.
Providers can explore certified vendors, industry associations, trade shows, online directories, and healthcare IT marketplaces for integrated PMS-EHR solutions.