Are Illinois Medicaid denials, payer edits and underpayments slowing our revenue? HelloMDs delivers accurate, compliant medical billing services in Illinois designed to improve claim acceptance, accelerate reimbursement and recover underpayments annually.
Schedule a consultation
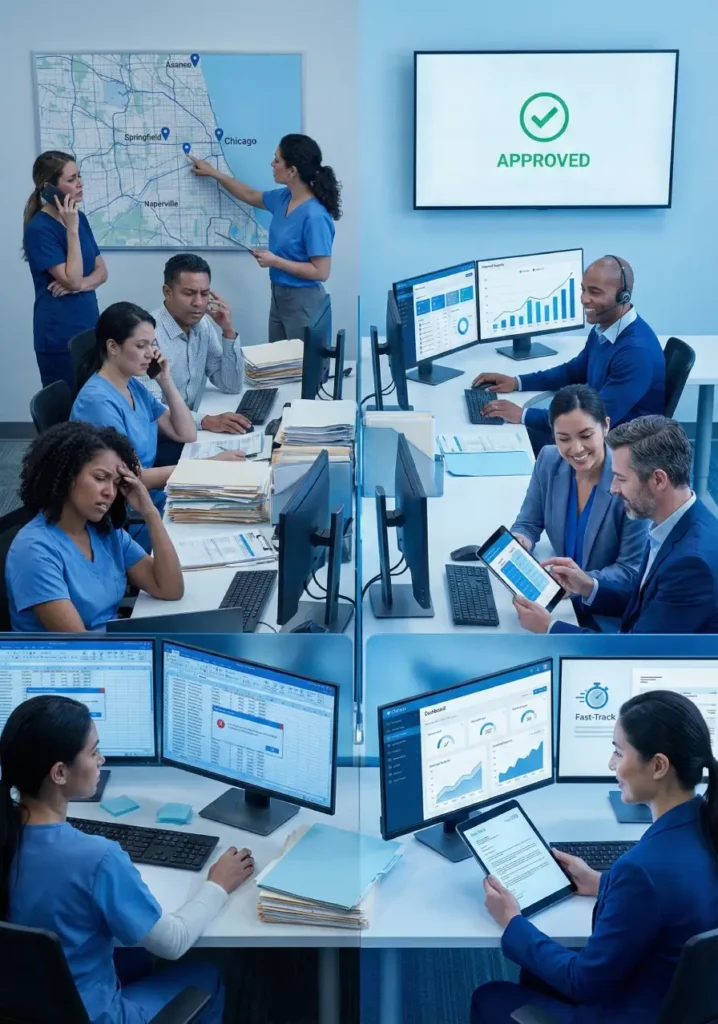
Practices across Chicago, Springfield, and Naperville lose 15-30% of potential revenue annually due to preventable mistakes. Illinois Medicaid’s specific documentation requirements reject claims that would pass in other states. Blue Cross Blue Shield IL and UnitedHealthcare each have unique modifier rules for codes like 99213, 99214, causing unexpected denials. Prior authorization delays for procedures including 70450 (CT head), 73721 (MRI knee), and J1745 (infliximab infusion) create revenue gaps averaging $12,000-$18,000 monthly.
Our Illinois-Specific Solutions:
AAPC-certified coders assign accurate ICD-10, CPT, and HCPCS coding across specialties.
Pre-visit eligibility checks with Illinois Medicaid, Medicare, BCBS IL, UnitedHealthcare, and Aetna confirm coverage, deductibles, copays, and authorization needs.
Electronic submission within 24 hours to the Illinois Department of Healthcare and Family Services and commercial payers with advanced error scrubbing.
We analyze root causes, correct documentation, and resubmit within 48 hours to recover revenue and reduce future denials.
Systematic collection of aging accounts. We contact payers daily via phone and portal until payment posts.
Daily EOB posting with automatic comparison against contracted rates. We catch underpayments immediately and file correction requests, recovering thousands annually.












Deep knowledge of Illinois Medicaid and state payer nuances that general billing partners miss.
Our coders and billers maintain up-to-date training on CPT, ICD-10 and state payer rule changes.
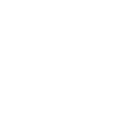
24/7 secure portal showing AR aging, claim status, denial rates by payer, collection percentages, and revenue trends for informed decisions.
Claims submitted within 24 hours versus the 3-5 day industry average. Faster submission means faster payment and reduced timely filing risks.

Eliminate billing staff salaries, payroll taxes, insurance costs, software licenses, and recruitment expenses when staff leave.

Encrypted transmission, secure cloud storage, multi-factor authentication, regular audits, annual staff training, and business associate agreements meeting federal requirements.

Illinois billing expertise and aggressive follow-up increase collection rates on billable services.

Fast submission and proactive follow-up reduce days in receivables from 45-60 days to 28-35 days, improving cash flow.

Certified coding and claim scrubbing reduce denials from the 10-15% industry average to 3-5% on initial submissions.

Real-time dashboards show claim status, AR aging, denial patterns, and payer performance for strategic decision-making.
No recruiting, hiring, training, or replacing billing employees. No payroll taxes, benefits, or continuing education expenses.
We verify contracted rates, catch underpayments, file reconsideration requests, and recover every dollar owed per contract.
Complete patient registration with insurance verification through the Illinois Medicaid portal or commercial payer systems, confirming active coverage and benefits.
AAPC-certified coders review documentation and assign accurate ICD-10 and CPT codes with required modifiers, ensuring medical necessity linkage.
Advanced claim scrubbing identifies errors before submission. Clean claims are transmitted electronically within 24 hours to all payers.
Daily payment posting with automatic reconciliation against contracted rates. Underpayments are flagged immediately for correction requests.
Denied claims are analyzed for root cause. We correct errors, gather documentation, write appeal letters, and resubmit within deadlines.
Systematic AR follow-up with phone calls to payers, portal tracking, and escalation procedures until full payment is received.
Our Illinois clinic struggled with denied Medicaid claims and telehealth billing confusion. HelloMDs implemented precise ICD-10 and CPT coding, resolving all denials within two months.
Outsourcing medical billing reduces staff costs, improves claim accuracy, and increases collections. Certified coders handle CPT codes (e.g., 99213, 99214), ICD-10 codes (e.g., E11.9, M54.5), and HCPCS codes (e.g., J1745) to ensure compliant submissions and faster reimbursements.
In-house billing often leads to missed claims, coding errors, delayed payments, and compliance risks. Practices may struggle with CPT, ICD-10, and HCPCS coding accuracy, Medicaid documentation requirements, and payer-specific edits.
Look for AAPC-certified coders, experience with Illinois Medicaid, and knowledge of CPT, ICD-10, and HCPCS codes. Ensure the service offers denial management, AR follow-up, prior authorization support, and real-time reporting.
Costs vary by volume and complexity. Most providers charge a percentage of collected revenue or a flat monthly fee. Services cover CPT (99213, 99214), ICD-10 (E11.9, M54.5), and HCPCS (J1745, 70450, 73721) coding, claims submission, and denial resolution.
Local billing services know Illinois Medicaid rules, payer edits, and documentation standards. They manage CPT, ICD-10, and HCPCS codes according to Illinois-specific guidelines, reducing denials and increasing timely reimbursement.
Key features include: AAPC-certified coding, CPT/ICD-10/HCPCS accuracy, denial resolution timelines, prior authorization support, AR follow-up, and HIPAA-compliant data management.
Switch when claims face repeated denials, underpayments, delayed reimbursements, or staff turnover. Accurate CPT, ICD-10, and HCPCS coding, along with AR management, ensures improved revenue flow immediately after switching.