Home / Dermatology Medical Billing
We know running a dermatology practice is not easy. It can be complicated for you if you are balancing patient care with insurance claims, coding accuracy, and revenue management simultaneously. When you get paid correctly and on time should not feel like solving a puzzle every day. However, many dermatology practices lose thousands of dollars annually due to coding errors, claim denials, or simply missing charges for procedures performed.
Dermatology medical billing is not like normal medical billing; it takes special know-how. Codes change often, each insurance company has its own rules, and even a small error can delay payment for weeks.
This guide walks you through everything you need to know about dermatology billing and coding, from understanding common procedure codes to choosing the right support for your practice.
Dermatology medical billing is the process of translating dermatology services like consultation, biopsies, excisions, Mohs micrographic surgery, and acne treatments into accurate claims submitted to insurance companies for reimbursement.
Billing for dermatology isn’t just about sending claims. It includes:
Dermatology medical billing is different from traditional medical billing because dermatology is more complex, as a single patient visit might involve multiple procedures a skin exam, biopsy and cryotherapy. All of these processes require their own code with specific modifiers. The accurate claims are important because when you don’t submit them correctly, it can lead to denial or delayed payments, longer accounts receivable times, compliance and audit issues
Did you know:
According to industry data, dermatology practices face denial rates ranging from 5% to 15%, often due to coding specificity issues. That’s significantly higher than many other specialties. Having a specialized dermatology billing service can dramatically reduce these denials.
Mastering codes is key to successful dermatology medical billing and coding. CPT codes describe procedures, while ICD-10 codes pinpoint diagnoses. In 2025-26, updates from the AMA and CMS introduce refined codes for better specificity, like expanded subtypes for skin cancers.
Procedure/Diagnosis | CPT Code | ICD-10 Code | Description |
Tangential Biopsy (single lesion) | 11102 | L57.0 | Actinic keratosis biopsy for diagnostic sampling. |
Punch Biopsy (single lesion) | 11104 | L70.0 | Acne vulgaris punch for deeper tissue analysis. |
Destruction of Premalignant Lesion (first) | 17000 | L57.0 | Actinic keratosis: destruction of the first AK lesion (e.g., cryo, laser) |
Mohs Surgery (first stage, head/neck) | 17311 | C44.311 | Basal cell carcinoma removal with microscopic control (linked to malignancy) |
Excisions (benign, 2.1-3.0 cm, trunk) | 11403 | L82.1 | Seborrheic keratosis excision with margins. |
Phototherapy (PUVA) | 96910 | L20.9 | Atopic dermatitis treatment of unspecified dermatitis with ultraviolet light. |
Matching ICD-10 for dermatology with CPT codes ensures clean claims. Common examples:
The connection between diagnosis and procedure codes must be clinically logical. For example, billing CPT 11102 (skin biopsy) with ICD-10 L70.0 (acne) would likely trigger a denial unless the biopsy was unrelated to the acne diagnosis.
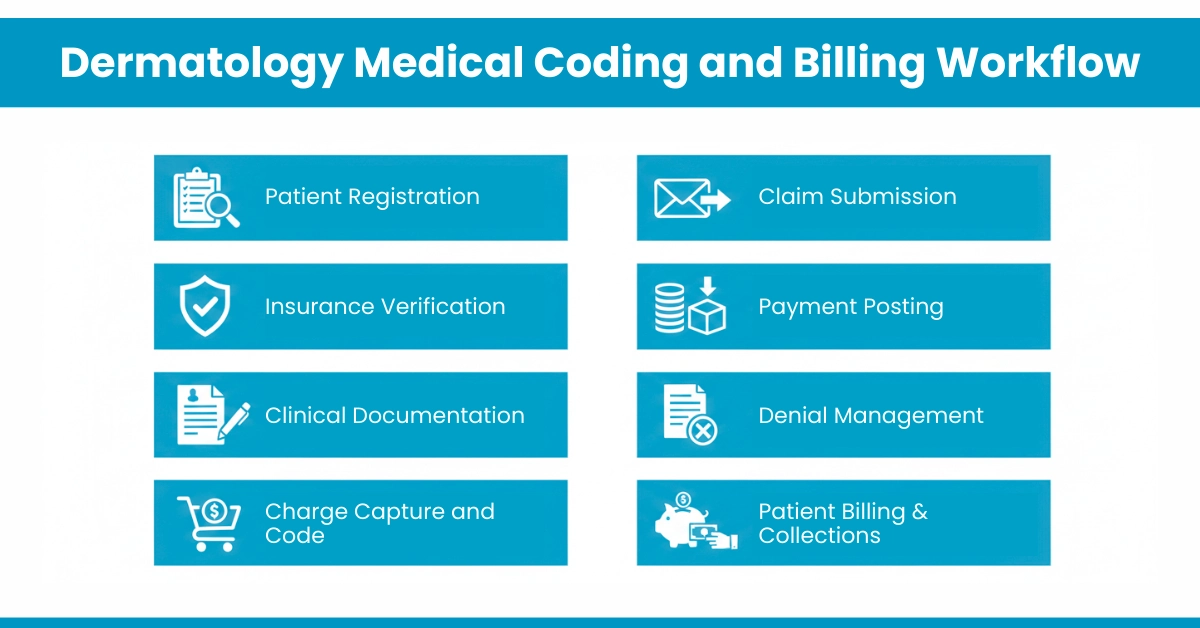
A well-structured workflow ensures that clinical services translate into clean, approvable claims. Here’s the essential process:
Before the patient arrives, verify insurance eligibility and secure prior authorizations for procedures like biopsies or specialized treatments.
Provider must document:
Our in-house Certified dermatology medical coders translate documentation into accurate codes. This step requires specialized knowledge. General coders often miss dermatology-specific nuances. Charge entry services must capture every billable procedure, including supplies and pathology referrals
Submit clean claims electronically with proper modifiers. For example, modifier -59 indicates distinct procedural services, crucial when performing multiple procedures during one visit.
Payment posting provides insights into reimbursement trends, helping identify underpayments.
Analyze causes of denials and resubmit corrected claims.
Manage patient balances and offer payment options.
Understanding specialty billing processes is key to accurate reimbursements. For insights into general billing workflows and CPT/ICD coding best practices, check out our guides on types of medical billing and CPT Code 97530 for therapeutic activities. These resources can help dermatology practices streamline claims and reduce denials
At Hello MDs, our AAPC-certified experts handle this end-to-end, ensuring your dermatology billing performance stays top-notch without overwhelming your team.
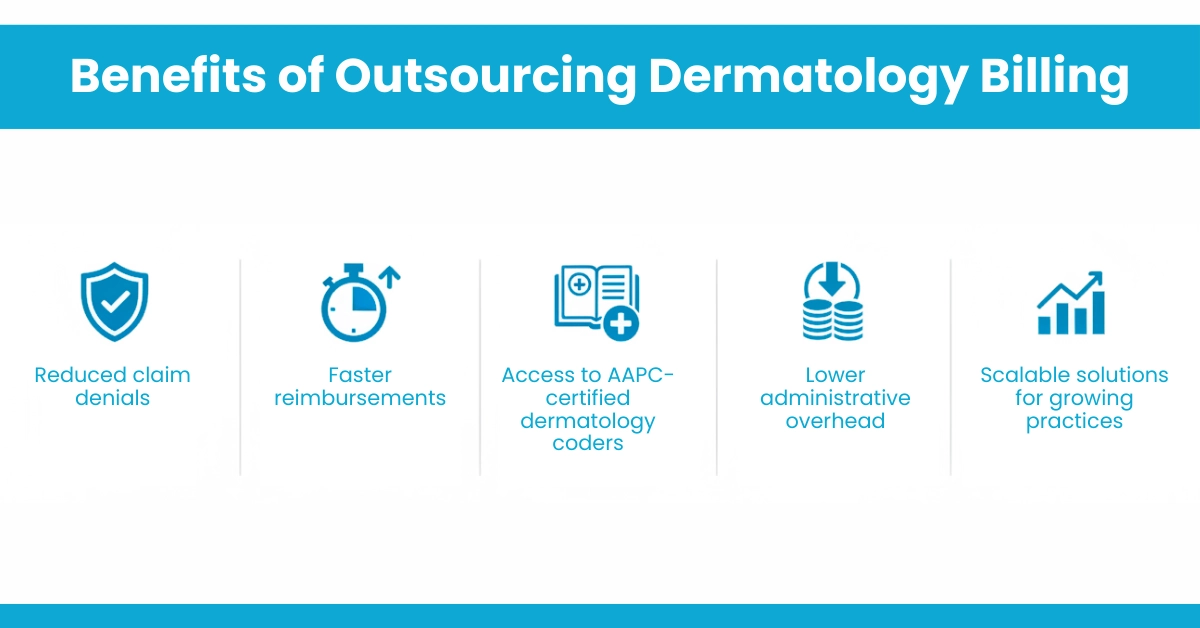
Many practices struggle with in-house billing due to staffing shortages, training costs, and increasing payer complexity. Outsourcing to a dermatology medical billing company can be a strategic advantage.
Benefits of Outsourcing Dermatology Billing
What to Look for in a Billing Company
Whether you’re working with West Coast dermatology billers or a nationwide provider, specialization matters.
Patient affordability is a growing concern. Offering a dermatologist payment plan can improve collections while enhancing patient satisfaction.
Integrating Payment Plans with Billing Systems
Modern dermatology billing services integrate payment plans directly into billing workflows, ensuring accurate patient balances and timely collections.
Example Financial Workflow
When your billing system includes robust insurance eligibility verification, you catch coverage issues before they become collection problems. This proactive approach protects your revenue while maintaining patient trust.
To optimize dermatology RCM
Practices that invest in specialized billing support typically experience faster reimbursements and reduced operational strain.
Coding errors, missing modifiers, or incomplete documentation often lead to denied claims.
Incorrectly billing cosmetic procedures as medically necessary can cause denials or patient disputes.
Procedures like biopsies or excisions may be undercoded or not billed at all, leading to lost revenue.
Constant updates to CPT codes and payer policies make it difficult to stay compliant.
Unpaid or slow-paying claims increase AR days and disrupt predictable revenue.
Dermatology medical billing and coding isn’t just about submitting claims; it’s about understanding the nuances of dermatology procedures, payer policies, and documentation standards. Whether you handle billing in-house or partner with specialized dermatology billing services, the fundamentals remain the same: accurate coding, thorough documentation, prompt claim submission, and persistent follow-up.
By applying the correct CPT and ICD-10 codes, documenting medical necessity, and seeking expert support from dedicated billing services like those offered by Hello MDs, dermatology practices can reduce denials, streamline RCM, and improve financial sustainability.
Disclaimer:
This information is for general understanding only and is not medical or billing advice. Always check codes with official guidelines or certified experts. The visuals present in the content are AI-generated for example purposes only.
Reputable organizations like AAPC, AHIMA, and specialty billing companies offer dermatology-focused billing and coding training programs.
Outsourcing is ideal when denial rates rise, staff lack expertise, payments are delayed, or the administrative workload affects patient care.
Practices should update billing procedures annually, or whenever CPT, ICD-10, payer rules, or compliance regulations change.
Dermatology-specific billing companies with AAPC-certified coders like HelloMDs specialize in accurate dermatology coding, billing, compliance, and denial management.