In medical billing and insurance claims processing, it is important to understand the PR 204 Denial Code. Basically, it is a common code that occurs when a service, medication, or test is denied or is not covered under the patient’s insurance plan. This means the patient is responsible for paying the cost. Don’t worry, we know that this is so frustrating for health care providers. Because of the delays in payments and also increased administrative work.
In this guide, we’ll explain what the PR 204 Denial Code is. What does it mean, the common reason behind it, and also give you a step-by-step procedure to solve this problem with the best solution, HelloMds. You will also learn about how medical billing services can help you reduce these denials and improve your insurance reimbursements. At HelloMDs, our team of AAPC-certified billing experts and RCM professionals helps you to handle such denials efficiently.
The PR 204 Denial Code stands for:
“Services, equipment, or drugs not covered under the patient’s insurance plan.”
The 204 denial code is part of the Claim Adjustment Reason Codes (CARC) system, and the word PR stands for Patient Responsibility. When we explain this in other words, like when you see these types of denials, it means that the patient is financially responsible for the charges. This is because their insurance plan doesn’t cover billing services.
This code is often used for:
Understanding this code is crucial for preventing repeated denials and ensuring claims are properly processed.
When you know about PR denial codes, it becomes easier for healthcare providers and the medical billing team. They figure out the problems why your claims were denied and what you do next. The table below shows some common PR codes that tell you the meaning, why they happen, and how to handle them accurately with medical billing services. This will help to make a quick and fast decision to resolve denied claims faster.
Denial Code | Meaning | Common Reasons | Recommended Action |
PR 204 | Services not covered by the patient’s plan | Service excluded, out-of-network provider, lack of prior authorization | Verify coverage, educate the patient, and appeal if applicable |
PR 205 | Patient deductible not met | The remaining deductible is not satisfied | Inform the patient, collect the deductible |
PR 307 | Patient copay or coinsurance required | Copay not collected at the time of service | Bill the patient promptly, confirm the payment plan |
CO 45 | Charges exceed the fee schedule or maximum allowed | Contracted rate lower than the billed amount | Adjust claim, re-bill according to contract |
OA 222 | Duplicate claim submitted | Same service billed multiple times | Verify claim history, resubmit corrected claim |
PR 130 | Non-covered services | Elective procedures, experimental treatment | Verify plan exclusions, inform the patient before service |
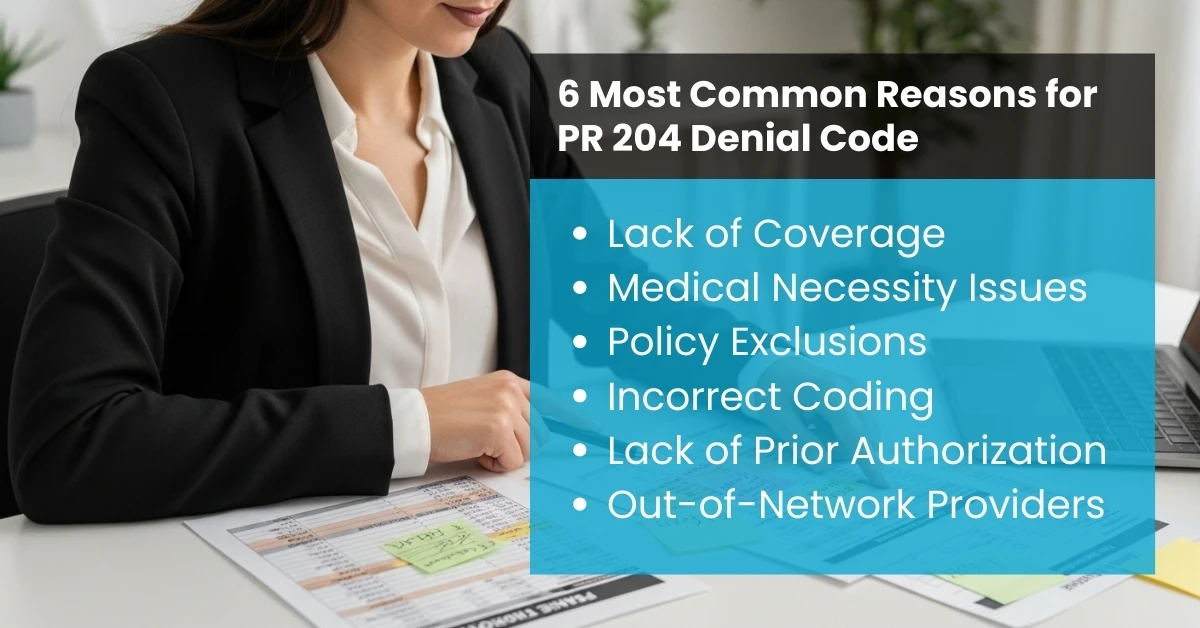
Here are some of the most frequent reasons claims are denied with this code:
The most common reason is that the patient’s insurance plan simply doesn’t cover the billed procedure, test, or equipment.
Insurance carriers may deny claims if they determine the service was not medically necessary based on the patient’s records.
Certain treatments, medications, or equipment are specifically excluded in the policy contract, making the patient responsible for these costs.
If the procedure or diagnosis code doesn’t match the medical necessity documentation, the claim may be denied.
Some services require pre-authorisation. Failure to obtain this leads to automatic denial.
If the provider is out-of-network, the insurance may reject the claim under PR 204.
Resolving PR 204 denials requires a step-by-step process to identify errors, appeal claims, and ensure accurate medical coding and billing in the future:
Use Hello MDs’ eligibility verification services to confirm the patient’s insurance plan details before scheduling services. Check coverage for tests, drugs, and procedures.
Ensure documentation supports the medical necessity of the service. Include supporting clinical notes in claims.
Use accurate CPT and ICD-10 codes that align with insurance payer policies. Incorrect codes often trigger denials.
For high-cost services, verify prior authorization requirements. Always document approval numbers.
If you believe the denial is incorrect, file an appeal submission process with additional documentation, such as medical records and policy references.
Our team also offers patient financial counselling to clarify out-of-pocket responsibilities, ensuring transparency and timely payments.
Dealing with claim denials like PR 204 can be time-consuming for medical practices. This is where Revenue Cycle Management (RCM) services and medical billing companies like Hello MDs play a vital role in minimising denials and improving healthcare claims processing. Here’s how they help:
Medical billing experts use advanced software to verify insurance coverage and detect potential policy exclusions before claims are filed. This prevents PR 204 denials upfront.
Billing specialists ensure that all services are coded correctly using CPT, ICD-10, and HCPCS codes. They review documentation to support medical necessity, reducing denials caused by claim submission errors.
Medical billing teams track and secure pre-approvals for services that require authorization, ensuring smoother claim approvals.
If a claim is denied, billing professionals handle appeals and resubmissions. They know exactly how to communicate with insurance payers and provide the right evidence to overturn denials.
Medical billing services analyze denial code categories to pinpoint the root causes of repeated PR 204 denials and implement long-term solutions.
Billing teams educate patients about their coverage, expected costs, and accounts receivable (A/R) responsibility to avoid payment disputes.
By partnering with Hello MDs, healthcare providers can reduce administrative workload, increase claim approvals, improve health insurance reimbursement, and revenue cycle management (RCM).
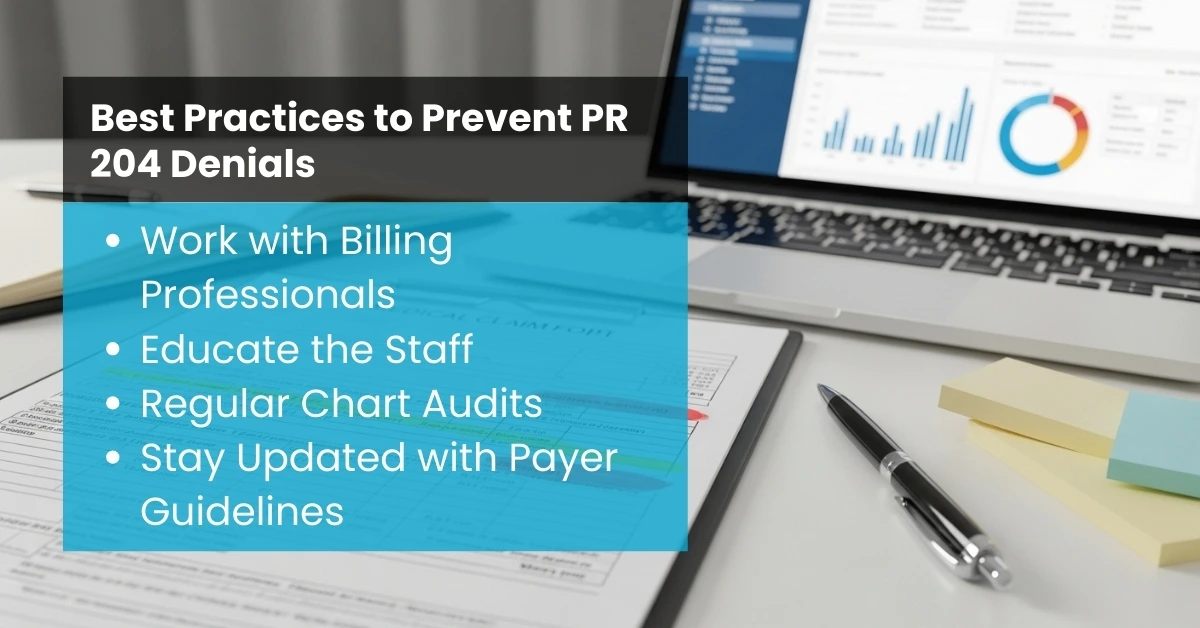
To avoid frequent PR-204 denials, healthcare providers should implement these best practices—something HelloMDs specializes in to streamline billing and improve revenue cycle efficiency:
The PR 204 Denial Code shows that a service, medication, or device isn’t covered under the patient’s insurance plan. So don’t worry, it is a common denial; you can avoid these denials and minimize them. If you understand what the PR 204 denial code means, it makes it easier for your healthcare provider and billing team to resolve your issue quickly and efficiently.
Medical billing services play a crucial role in addressing PR 204 denials. They properly ensure that the documentation is correct, manage your prior authorizations, and also handle the appeal submission process. Healthcare providers who use professional billing support often experience higher claim acceptance rates and improved accounts receivable (A/R) and health insurance reimbursement.
Not always. Even though PR 204 means the patient is responsible, some denials happen because of outdated information or insurance errors. Updating patient details or reaching out to the insurer can sometimes fix it. HelloMDs can help with eligibility checks and denial management to sort this quickly.
Yes! PR 204 is a denial, not a rejection. This means it can be appealed with proper documentation. HelloMD’s billing and appeal services can guide providers step by step to maximize reimbursements.
Yes. The claim went through but was denied. Unlike rejected claims, which never reach processing, PR 204 needs attention to recover the payment.
PR 204 denials can cause big revenue losses if not handled. With the right process, like reviewing claims and communicating with patients, these losses can be reduced. HelloMD's RCM services help prevent these financial setbacks.
For Medicare, PR 204 usually comes with a note saying the service or item isn’t covered under the patient’s plan. The next step is often an appeal with the required documents. HelloMDs can help manage this entire process smoothly.
Some simple steps include:
HelloMDs offers services for coverage verification, patient communication, and claim management to help avoid PR 204 denials from happening in the first place.