Accuracy in medical coding is more than just a formality; it is essential for proper documentation, billing, compliance, and maintaining revenue flow. Hyperlipidemia is one of the most prevalent conditions in medical practice, particularly in internal medicine, family medicine, and cardiology practices.
Hyperlipidemia, also known as dyslipidemia or high cholesterol, is not only a health issue but also a billing and coding problem when not recorded properly. ICD-10 code for Hyperlipidemia (E78.5) is common throughout the U.S.; numerous practices are getting claims denied due to the lack of specificity in the coding process.
In this guide, we will explain hyperlipidemia ICD-10 codes, documentation, medical billing processes, credentialing, payer-related specifications, and prevent expensive denials.
Hyperlipidemia is a metabolic condition in which an excessive amount of fat is present in the body, such as cholesterol or triglycerides. It is common that most patients do not have the symptoms at first. If a patient doesn’t treat the hyperlipidemia, this causes atherosclerosis, cardiovascular disease, and stroke.
Pro Tip for Coders: Always encourage providers to document the type of hyperlipidemia instead of defaulting to unspecified (E78.5). Specific coding improves payer acceptance and helps practices avoid claim audits.
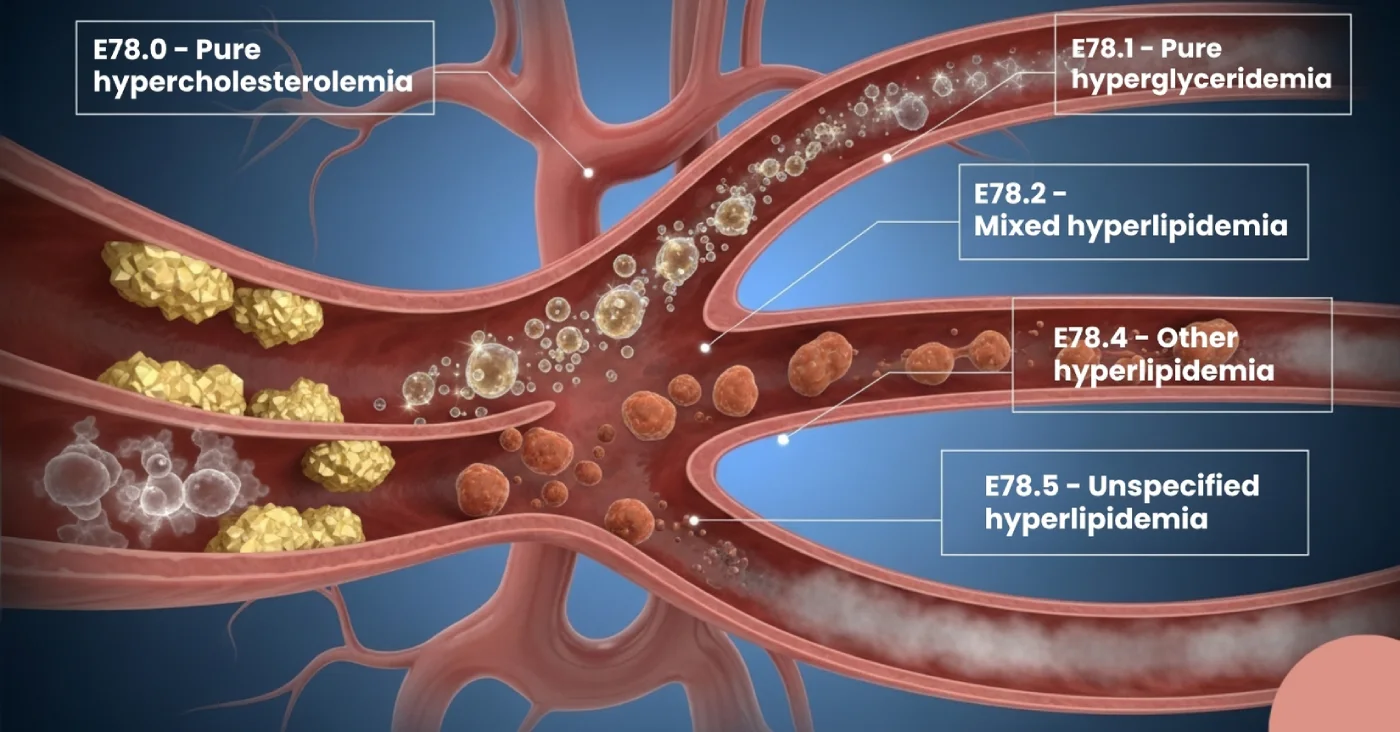
The ICD-10-CM coding system places hyperlipidemia under Chapter 4: Endocrine, Nutritional, and Metabolic Diseases.
For medical billers and coders, hyperlipidemia coding directly impacts revenue cycle performance. Here’s how:
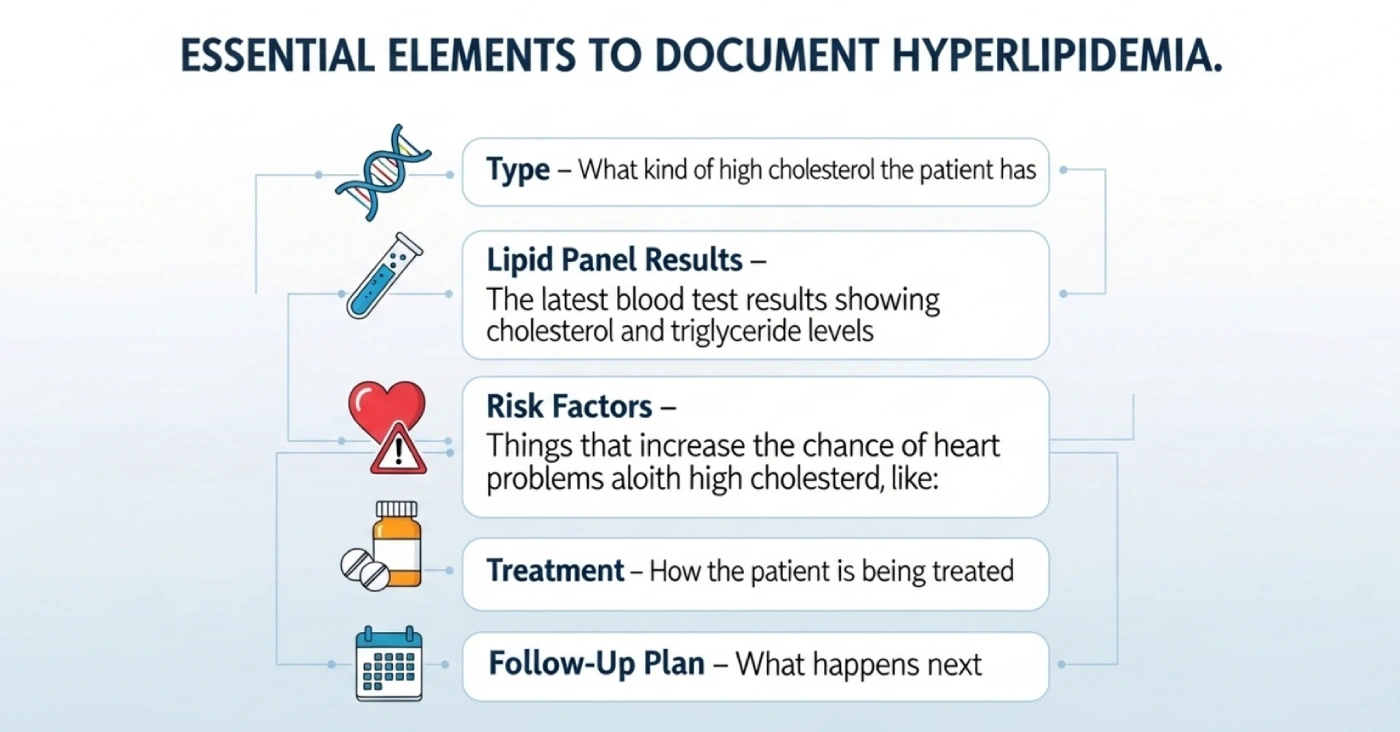
To ensure that claims for hyperlipidemia are paid without issues, providers should follow strong clinical documentation improvement (CDI) practices. Repeated use of E78.5 without lab specificity is a top reason for lab claim denials, particularly under Medicare Advantage and commercial plans.
Example of weak documentation:
“Patient has high cholesterol.” (Not specific enough for coding).
Example of strong documentation:
“Patient diagnosed with mixed hyperlipidemia (E78.2). LDL: 160 mg/dL, triglycerides: 250 mg/dL. Started atorvastatin, advised dietary changes, follow-up in 3 months.”
Strong documentation gives coding accuracy, payer compliance, and also reduces denials.
Even the best coding won’t help if the provider is not credentialed with the payer. Credentialing ensures the provider is authorised to bill Medicare, Medicaid, or commercial insurance.
Example: Medicare can provide lipid panels on an annual basis to patients who have cardiovascular risk factors, but commercial insurers can offer them more often in accordance with the clinical need.
In the case of clinics and solo practitioners, outsourcing medical billing and credentialing can be an effective solution to have claims of hyperlipidemia and other chronic conditions approved within a short duration without the administrative hassle.
Hyperlipidemia often does not exist in isolation; it’s commonly linked to other chronic diseases. Coding these correctly improves risk adjustment scoring and supports medical necessity.
Insurance companies and CMS conduct audits to detect upcoding, undercoding, or misuse of unspecified codes. Overusing E78.5 can be a red flag.
Maintaining compliance protects your practice from denials, takebacks, and legal issues.
What appears to be a very straightforward code, hyperlipidemia (ICD-10 code E78.5), has a significant impact on medical billing and credentialing. Clean claims, fewer denials, and stable performance of the revenue cycle can be achieved through proper documentation, coding to specificity, and payer compliance.
Hello MDs assists medical facilities in medical billing, credentialing, and revenue cycle management (RCM). Our experts help ensure accurate coding, payer compliance, and faster reimbursement, so your team can focus on delivering high-quality patient care.
The major code is E78.5- Hyperlipidemia, unspecified, of abnormal lipid levels. In case detailed information is known, specific codes must be applied such as E78.0 (pure hypercholesterolemia).
CPT 80061 is used in the lipid panel test, which is usually associated with E78.x codes. This is a test that is used to determine cholesterol and triglycerides to determine the level of lipid-related conditions.
Yes, hyperlipidemia may be listed as the principal diagnosis in case it is the primary cause of the visit. Its use in claims is supported by the proper documentation of symptoms or related conditions.
The two terms refer to abnormal lipid levels though E78.5 is normally applied in the billing of hyperlipidemia.
Dyslipidemia can include more extensive lipid disorders, but ICD-10 prefers codes of hyperlipidemia.
The code is E78.0, used when a patient has high cholesterol without other lipid abnormalities.
R29.6 is not related to hyperlipidemia; it is the code for “Repeated falls.”
The main term is “Hyperlipidemia, unspecified,” which corresponds to the ICD-10 code E78.5.