Home / How Many Types of Medical Billing
Medical billing is a crucial part of running a successful healthcare practice. For providers, understanding the types of medical billing is not just about getting paid—it’s about ensuring accuracy, compliance, and smooth revenue cycle management (RCM). With healthcare billing becoming more complex due to evolving insurance requirements, coding standards, and payment models, knowing the billing methods available can help streamline your operations and maximise reimbursements.
In this blog, we’ll explore how many types of medical billing exist, what makes them different, how your practice can benefit from the right billing model, and how Hello MDs helps you in this regard.
Medical billing is the process of translating patient care services into claims for insurance reimbursement or direct payment. It involves:
Medical billing is different from medical coding, though they are closely connected. While coders assign accurate diagnostic and procedural codes, billers use those codes to generate and submit claims.
Choosing the right billing method impacts:
Whether you run a solo practice, a multi-speciality clinic, or a hospital, understanding billing types helps you select the best system for your needs.
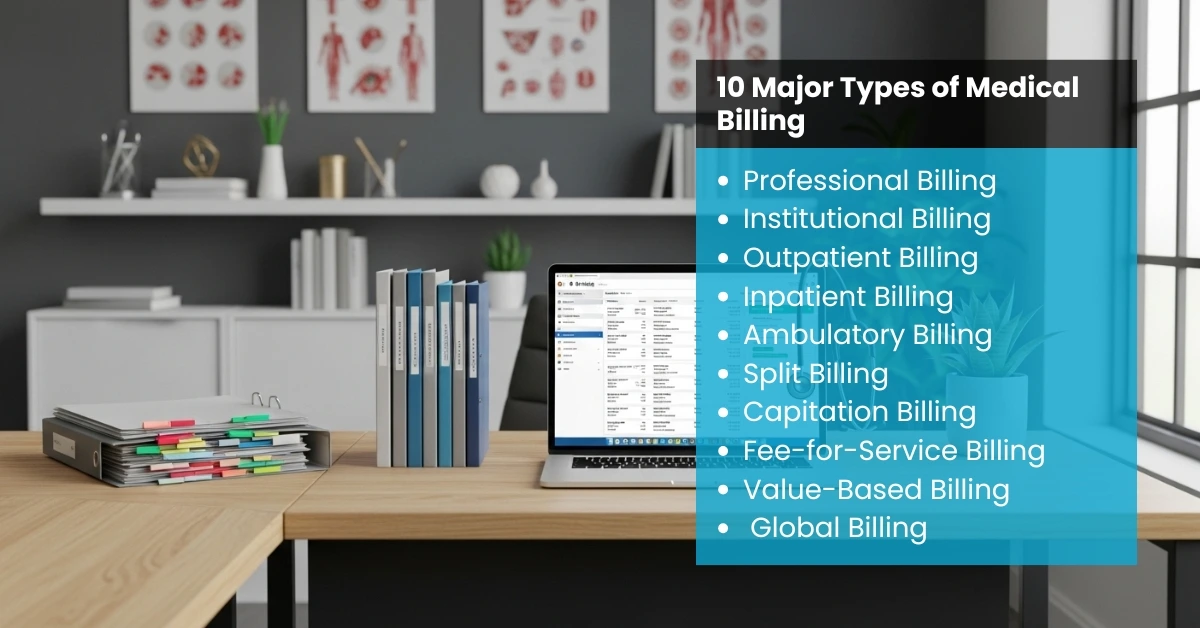
There are several types of medical billing, and each serves a specific purpose in the healthcare industry. Here’s a detailed breakdown:
Professional billing is used for individual practitioners or small outpatient services. Claims are submitted using CMS-1500 forms. This model suits private practices and specialty clinics.
Institutional billing covers hospitals, nursing facilities, and rehab centers. Claims are submitted on UB-04 forms, which include more data about inpatient care, equipment, and facility services.
Outpatient billing is for patients who receive treatment but don’t stay overnight. Examples include physical therapy sessions, imaging scans, and outpatient surgeries.
Inpatient billing covers patients admitted for longer stays, often involving multiple providers, medications, and extended care services.
Ambulatory billing is specific to same-day procedures performed at ambulatory surgery centres (ASCs) or speciality clinics.
Split billing divides charges between primary insurance, secondary insurance, and patients. This is common in scenarios involving multiple payers.
In capitation billing, providers receive a fixed monthly payment per patient, regardless of services rendered. This model is popular in managed care.
A traditional billing model where providers charge for each service. While it maximises revenue, it can create administrative challenges.
Value-based billing rewards providers for patient outcomes rather than service quantity. It’s part of a healthcare shift toward quality-driven care.
Global billing applies a single charge for an entire episode of care, such as maternity packages or surgical care bundles.
Understanding the medical billing process is essential for any healthcare provider aiming to streamline revenue collection and reduce claim denials. Each step in the process plays a crucial role, from patient registration to payment posting, ensuring accuracy and compliance. The following table breaks down the key steps in medical billing, along with the tools and entities involved:
Step | Description | Key Entities/Tools Used |
1. Patient Registration | Collect patient demographics, insurance details, and verify eligibility. | Practice Management System, EHR, Insurance Verification. |
2. Medical Coding | Assign accurate codes for diagnoses and procedures. | ICD-10, CPT, HCPCS Codes. |
3. Claim Creation | Compile codes and patient details into a formal claim. | CMS-1500 (Professional) or UB-04 (Institutional) Forms. |
4. Claim Submission | Send claims electronically or on paper to payers. | Clearinghouses, EDI Submissions. |
5. Payer Adjudication | Insurance companies review claims and approve or deny them. | Payer Portals, Automated Adjudication Systems. |
6. Payment Posting | Post insurance payments, adjustments, and patient balances. | Billing Software, A/R Reports. |
7. Denial Management | Resolve claim denials or rejections (e.g., PR-204 denial). | Denial Codes, Claim Correction Tools. |
8. Patient Billing & Collection | Send statements and collect outstanding balances. | Patient Portals, Payment Gateways. |
Regardless of the billing type, a smooth process ensures accurate reimbursement:
Modern billing systems rely heavily on technology:
Selecting the right billing approach depends on:
For small practices, professional billing is efficient, while institutional billing suits larger facilities. Practices embracing value-based care may shift toward global or value-based billing models.
Medical billing is prone to challenges like:
Healthcare billing is evolving with technology and policy changes:
At Hello MDs, we specialize in providing end-to-end medical billing and RCM services for healthcare providers, clinics, and hospitals. Our team ensures:
By outsourcing your medical billing to HelloMDs, you gain a dedicated team of certified billing specialists who help maximise your revenue while keeping your practice compliant and efficient.
Understanding how many types of medical billing exist is essential for optimizing your practice’s financial health. From professional billing for small practices to institutional billing for large facilities, choosing the right system reduces denials, improves patient satisfaction, and streamlines revenue.
If you’re ready to simplify your billing process, Hello MDs offers a proven solution to make your practice more profitable and stress-free.
Professional billing is for individual providers; institutional billing is for hospitals and facilities.
There are at least 10 recognized types of billing, including outpatient, inpatient, and capitation billing.
It’s a traditional model where providers charge separately for every service rendered.
Providers are paid based on patient outcomes, incentivizing quality over quantity.
A clearinghouse is a platform that checks claims for errors before sending them to insurance companies.
It saves time, reduces claim denials, and ensures compliance.
Software depends on practice size, but leading solutions integrate with EHRs for automation.