If you’re a medical coder, biller, or provider, you’ve probably seen this: a claim for insomnia gets denied, and the reason? “Insufficient specificity” or “non-billable code used.” Sounds minor, but it adds up, delayed reimbursements, extra work, and lost revenue.
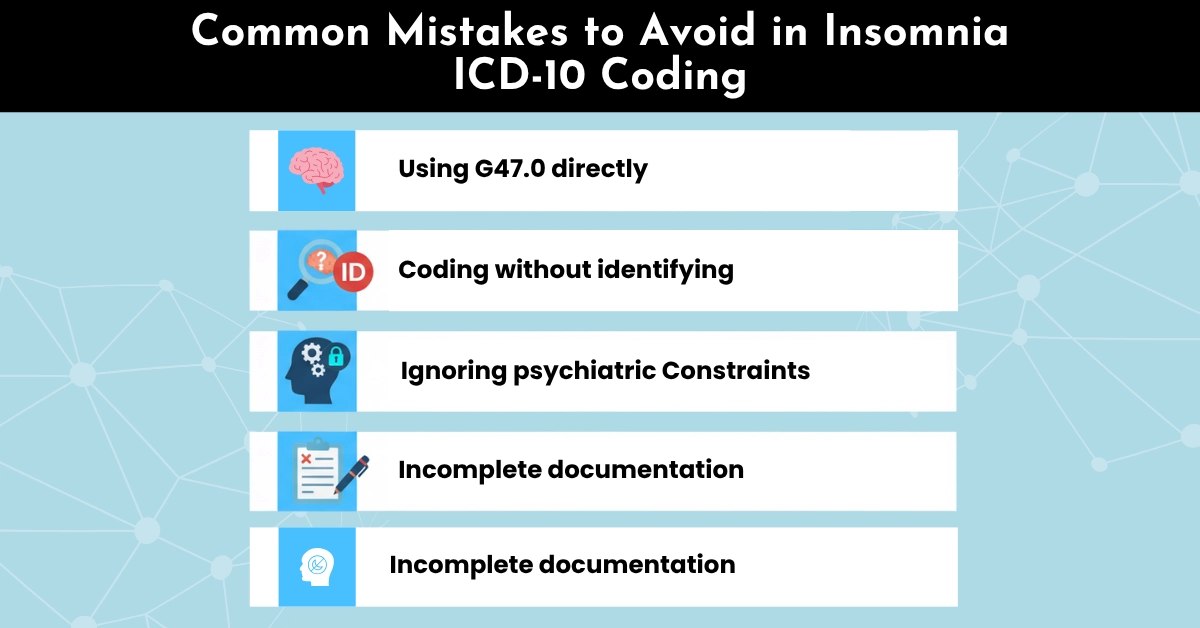
That’s because insomnia coding in ICD-10 isn’t just drop-and-paste. Between chronic vs. acute, primary vs. secondary types, plus the exclusions, combinations, and payer edits, it’s easy to miscode.
At Hello MDs, our AAPC-certified coders see this mistake all the time during coding audits. But the good news? It’s entirely fixable. In this guide, we’ll walk you through which insomnia ICD-10 codes to use, which to avoid, plus documentation best practices, payer nuances, and appeal strategies.
Insomnia is a persistent difficulty initiating, maintaining, or restoring sleep, despite opportunity and adequate conditions for sleep. Its symptoms include:
Clinically, insomnia may be acute, chronic, primary, or secondary to another disorder. Choosing the right classification is essential not just for patient care, but for accurate billing and payer acceptance.
Doctors use special codes, called ICD-10 codes, to record medical conditions for insurance and billing. Insomnia is grouped under G47.0, but this general code can’t be used on its own. Instead, your doctor will choose a more specific code, like G47.00 (unspecified insomnia) or G47.01 (insomnia caused by a medical condition), so your treatment and insurance claims are accurate.
That’s why accurate, detailed coding matters not just clinically but financially, and that’s where Hello MDs supports providers and coders.
The primary ICD-10 code for insomnia is found under F51.0 – Nonorganic Insomnia, with subcategories for more specific diagnoses. Providers must select the most accurate code based on the patient’s presentation.
Each code reflects the type of insomnia, helping payers and auditors understand the clinical reasoning for the patient’s care plan.
Understanding the cause and duration of insomnia is key to proper ICD-10 coding. Here’s how to break it down:
Note: This is not under the G47 family and is considered a psychiatric diagnosis.
You may also encounter Adjustment insomnia (F51.02) under certain mental health stressors.
Condition/Symptom | ICD-10 Code |
Sleep deprivation due to lifestyle | Z72.820 |
Stress-related lifestyle issues | Z73.3 |
Poor sleep hygiene | Z72.821 (if applicable, or document in provider notes) |
Fatigue | R53.83 |
Circadian rhythm disruption | G47.20 (Circadian rhythm sleep disorder) |
Z72.820 should not be used as a primary code for clinical insomnia (G47.00-G47.09 or F51.01). It can be used as a secondary or contributing factor based on documentation.
Example:
If insomnia is driven by lifestyle issues like chronic sleep deprivation (e.g., due to long work hours, poor sleep habits), Z72.820 may be reported as a contributing factor. However, it should never replace a primary insomnia diagnosis like G47.00 or G47.01.
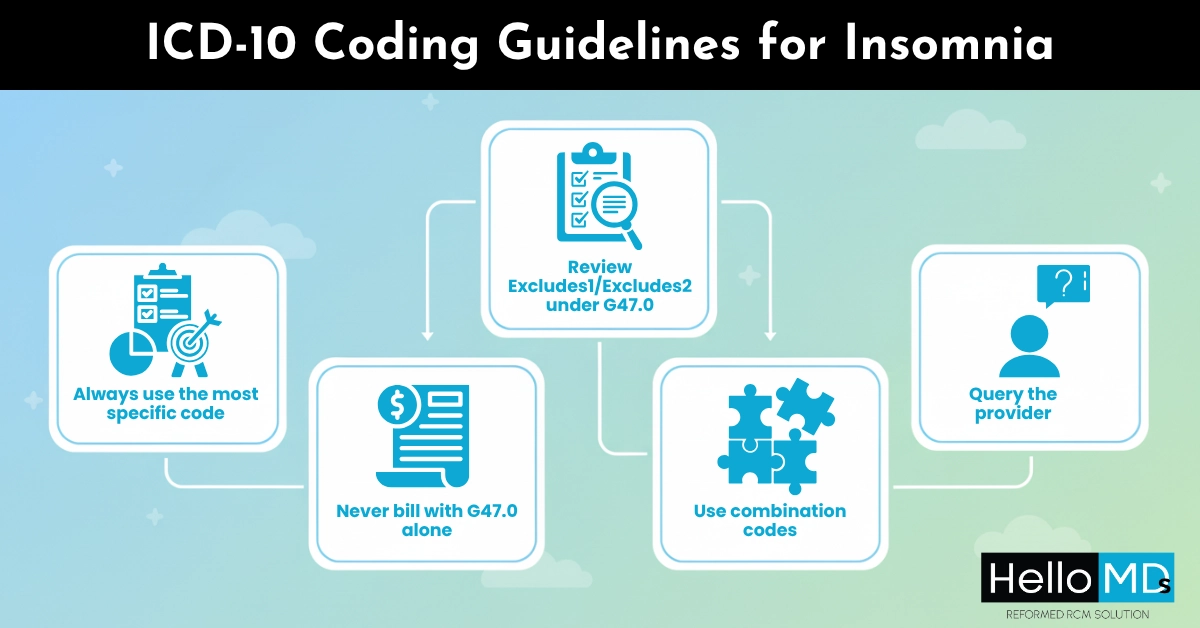
To ensure your insomnia-related claims are clean and compliant, follow these best practices:
Sleep disorders are often linked with chronic conditions like obesity, which also has specific ICD-10 codes. Explore our detailed guide on ICD-10 Obesity Codes
Without proper documentation, even the right ICD-10 code can result in denials. Here’s what you should include:
Patient reports insomnia lasting over 6 months. Associated with chronic lower back pain. Reports difficulty falling asleep and frequent nighttime awakenings. Diagnosed with insomnia due to chronic pain.
Correct Code: G47.01: Insomnia due to medical condition
Accurate ICD-10 coding is just one part. Pairing it with the correct CPT codes completes your claim:
CPT Code | Description |
99201-99215 | Office visits/outpatient consultations |
90834 | Psychotherapy, 45 minutes |
90847 | Family psychotherapy |
95810 | Polysomnography (overnight sleep study) |
99406 | Smoking cessation counseling (if linked to insomnia) |
Remember:
CPTs must align with medical necessity and documentation. Don’t forget the modifier and payer-specific requirements.
At HelloMDs, we help clinics and solo practices take the guesswork out of coding insomnia and every other sleep-related disorder. Our services go far beyond claim submission:
Let us handle the coding complexity so you can focus on patient care.
Insomnia may seem like a simple diagnosis, but coding it wrong can cost your practice time, money, and compliance risk. Now you know the critical distinctions between G47.00, G47.01, G47.09, and even F51.01, and more importantly, when and how to use them. When you document accurately, avoid exclusions, and code with intention, your insomnia claims don’t just go through. They pass cleanly, get reimbursed faster, and avoid unnecessary payer pushback.
At Hello MDs, we specialize in bridging the gap between clinical care and coding clarity. Whether you need a one-time insomnia code audit or full-service revenue cycle management, our AAPC-certified coders are here to help.
Contact Hello MDs today for a free insomnia coding review, and take one more step toward faster, cleaner revenue.
For informational purposes only, not medical or billing advice. Verify codes with official ICD-10 guidelines or certified professionals. Some images may be AI-generated or illustrative.
Yes, if insomnia and depression are separately diagnosed and documented. Use the F33.x for depression and a G47.x subcode for insomnia (unless insomnia is coded under F51 due to a psychiatric cause).
Use G47.01 if insomnia is clearly tied to a documented medical condition. Use G47.09 when insomnia is specified but not tied to a clear etiology.
Yes, if both are separately documented. Use F33.x for depression and appropriate G47.x or F51.x for insomnia.
Query the provider for details: duration, frequency, possible cause, or whether it’s primary or secondary insomnia.
G47.0 is a parent, non-billable code; payers reject claims using it without supporting specificity.
Yes, your procedure or therapy must be supported by diagnosis, medical necessity, and documentation to avoid denials.