Home / 99203 CPT Code
Understanding CPT codes is essential for healthcare providers, coders, and billing staff. Among the many CPT codes, 99203 is one of the most commonly used for new patient office visits. In this guide, we’ll explain everything you need to know about the 99203 CPT code, including documentation requirements, billing, insurance considerations, updates in 2025, and how Hello MDs will help you in this regard.
CPT code 99203 belongs to the category of Evaluation and Management (E/M) services. Specifically, it is used for new patient outpatient office visits. According to the American Medical Association (AMA) and the Centers for Medicare & Medicaid Services, a new patient is defined as someone who has not received professional services from the physician or another physician of the same specialty in the same group within the past three years.
This type of code represents a moderate-complexity visit. Healthcare providers use it when they need to perform a comprehensive evaluation and make medical decisions that are of moderate complexity.
Related codes include 99202, 99204, and 99205, which represent different levels of new patient E/M visits, varying by complexity and time spent.
For a 99203 visit, documentation must include:
The history should cover chief complaint, history of present illness, review of systems, and past/family/social history. The physical exam typically involves a detailed examination of multiple organ systems.
MDM is a crucial component of 99203. It includes:
Providers can also code based on time if the time spent face-to-face with the patient meets CPT guidelines. Correct documentation is key to supporting MDM or time-based coding.
When billing 99203, providers must consider:
Accurate coding ensures proper insurance claims processing and timely reimbursement.
To prevent claim denials or audits:
Regular auditing and training for coding staff help maintain compliance and efficiency.
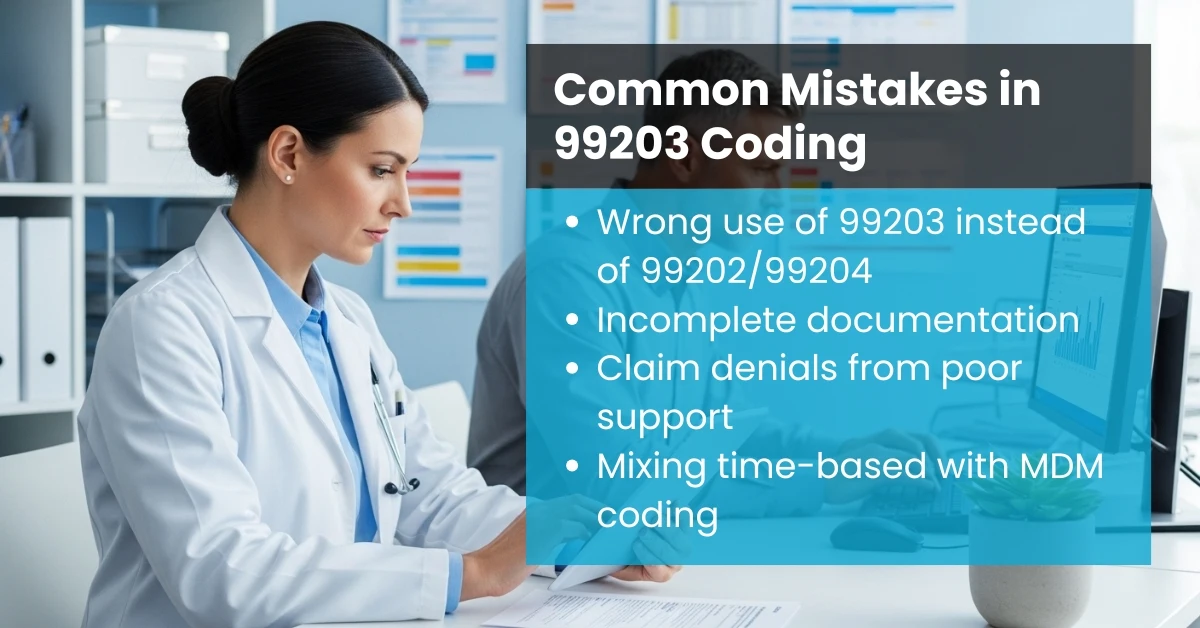
Errors in coding can lead to delayed or denied payments. Common mistakes include:
Being vigilant about documentation and coding compliance reduces these errors.
It’s important to differentiate 99203 from other new patient CPT codes:
CPT Code | Description | Complexity |
99202 | New patient, straightforward or low-complexity | Low |
99203 | New patient, moderate-complexity | Moderate |
99204 | New patient, moderate-to-high complexity | Moderate-High |
99205 | New patient, high complexity | High |
Time-based coding vs MDM-based coding can also affect which level is appropriate. Providers must evaluate both time spent and medical decision-making complexity before assigning a code.
CPT codes are updated annually. Key 2025 updates include:
Providers should stay updated with the CPT code updates and AMA guidelines to ensure accurate billing.
CPT code 99203 is a critical code for new patient office visits with moderate complexity. Proper understanding of documentation, medical decision making, billing, and insurance reimbursement is essential for healthcare providers, coders, and RCM teams. By following coding compliance, auditing best practices, and 2025 updates, you can ensure accurate claims, proper reimbursement, and improved revenue cycle efficiency
Yes, nurse practitioners (NPs) and physician assistants (PAs) can bill 99203 for new patient visits within their scope of practice. However, the visit must meet all documentation and complexity requirements for a moderate-level E/M service.
Reimbursement varies by payer, location, and provider type. For Medicare, 99203 typically reimburses at a moderate rate compared to lower-level codes like 99202, while commercial insurers may pay more depending on contract terms.
99203 is for new patients, whereas 99213 is for established patients. Both represent moderate-complexity visits, but the distinction affects billing rules, documentation requirements, and reimbursement.
Yes, telehealth visits can be billed as 99203 if the visit meets the same history, exam, and MDM requirements as an in-person visit. Some payers may require specific modifiers to indicate telehealth.
Providers should document:
Modifiers may be required in certain cases, such as:
Yes, as long as the overall medical decision making is of moderate complexity and the documentation supports all complaints, 99203 can be used. Providers must ensure the visit meets the CPT guidelines for history, exam, and MDM.