What Is ERA in Medical Billing? Providers Guide By Hello…
Medical Billing What Is ERA in Medical Billing? Providers Guide…
At Hello MDs, we simplify billing for physicians, clinics, and hospitals with end-to-end medical billing and RCM solutions. As a full-service medical billing company, we focus on accuracy, transparency, and faster reimbursements — helping healthcare providers maximize revenue effortlessly.
Support: (469) 421-2777









Tired of Denials? Call !
Call now for a free consultation. HelloMD’s healthcare billing services team streamlines payer rules, coding audits, prior authorization, and reporting, without disrupting clinical workflows.
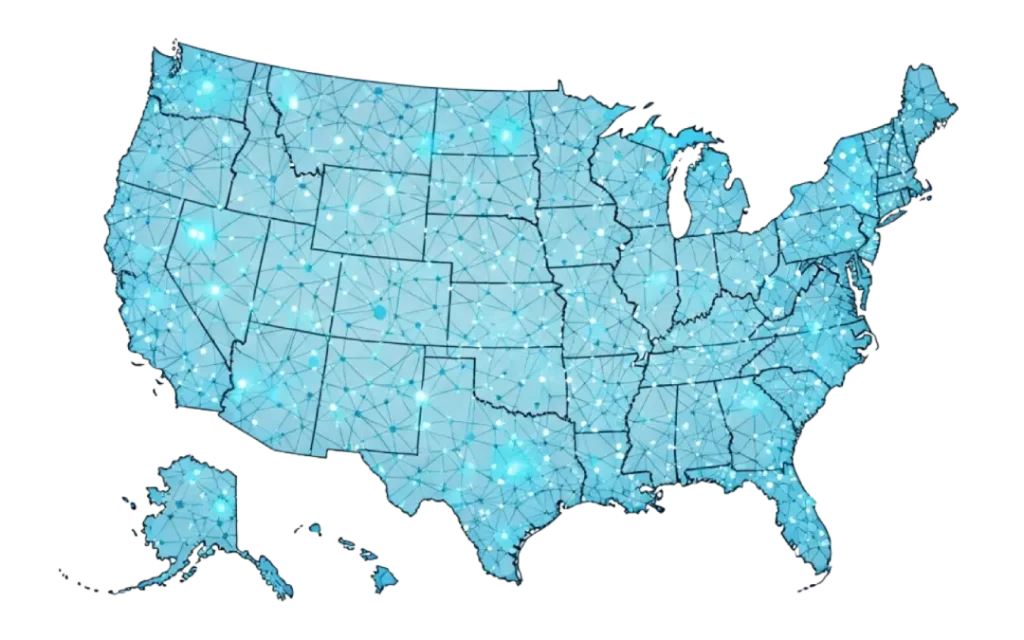
We are a professional medical billing and revenue cycle management (RCM) agency that operate not in only in Texas, California, Florida, New York, New Jersey, or Delaware but in nationwide. We offer comprehensive cost-effective medical billing solutions for all RCM process– from eligibility verification and claims submission to denial Management. Hello MDs ensuring your practice maximizes revenue with minimal hassle. In order to maintain the affordability factor, we offer affordable and flexible billing plans starting as low as 2.95% on Monthly Collections. Trusted by medical practices across the United States, our solutions deliver efficient, reliable, and fully optimized revenue cycle management for maximum financial performance.
Hello MDs offers end-to-end solutions for every type of healthcare provider from primary care clinics to specialty practices like cardiology, radiology, and orthopedics. Whether you’re running a small clinic, multi-specialty practice, or hospital, our full-service medical billing company covers every step of your revenue cycle.

We provide accurate and compliant medical coding related to your specialty by certified coders who ensure proper documentation and minimize claim errors

We take care of provider enrollment, payer credentialing, and contract updates along with handling complex paperwork, saving you time and administrative effort.

Our in house- team warmly identifies and resolves claim denials before they impact revenue by analyzing denial trends, correct root causes, and resubmit claims efficiently that helps you boost your claim acceptance rate.

Our team manages your aging account receivable with systematic approaches by using advanced hi tech collections software to track every unpaid claim efficiently
We Simplify your daily operations with customized management tools by automating scheduling, reporting, and billing for higher productivity.

We verify insurance coverage before patient visits to prevent claim issues with our system. It helps to check deductibles, copays, and plan limitations in real time smoother.

Behind every unpaid claim is a gap, and with years of training and hands-on experience in the medical billing industry, we know how to close it. We provide medical billing for all healthcare providers, medical specialists, and niche multi-site providers who need more than surface-level support. Our team handles prior authorizations, denial management, credentialing services, and full RCM healthcare services without disrupting your operations.
Unlike most medical coding and billing companies, we don’t stop at claim submission. We help gain payer access, reduce account ageing, and improve first-pass accuracy. As medical billing and coding experts, we understand how to manage your codes plus revenue flow without interruptions.
HelloMDs is your USA-based medical billing partner, with added support in digital marketing and virtual assistance. Reach out when your business needs billing and add-on assistance.
To be the most trusted medical billing company nationwide, delivering precise, human-led coding and credentialing services tailored to every medical speciality.

We remove billing complexity for physicians, clinics, and hospitals by providing scalable, process-driven medical coding and credentialing, built on accuracy.

From claim entry to payer follow-up, every workflow is engineered for medical billing companies needing speciality-specific alignment and full regulatory compliance.


Check our physician billing services reviews. We do what we do for consistent appraisal of reducing denials, improving cash flow, and freeing staff. Here’s what healthcare professionals are saying about working with us.
Overall, I think you guys are catching a lot of mistakes that we’ve made, and even mistakes that ECW made. So far, we’re really pleased with the services we’re getting — I haven’t seen any issues. Even though I don’t handle much of the billing side myself (I’m more on the clinical side), I can say that we’re definitely seeing more money in our pockets and not having to deal with denials and all of that. So far, we’re very pleased with everything.
The start to finish process with Hellomd was amazing. My main concern was onboarding and this was extremely well planned with no disruption's. A few months into the implementation I am learning all the missed opportunities that I am now capitalizing on. Would 100% recommend their services, I think I don't have to worry about any admin work moving forward! Thank you for a great experience and partnership!
It is a pleasure working with John ,Alex and their team for medical billing recover.They are sincere dedicated and hardworking and their team effort has benefited our organization tremendously not only with the recovery process but they have also pointed out flaws in our billing process and helped our biller rectify them.We thank you John and Alex for helping us and hope to keep our work relationship going. I recommend HelloMDs without reservation to my peers who need assistance with their billing.
Know When In-House Billing Costs You
Switch from in-house billing to guaranteed income. Use our calculator to see how outsourcing medical billing services in the US improves collections with HelloMD’s medical billing and coding solutions.

We manage the full billing lifecycle, code entry, claim filing, payer follow-up, and payment posting. Our medical billing credentialing services are end-to-end, and we even offer patient call support and digital marketing for doctors' services.
We cover billing, coding, prior authorization, denial appeals, account receivable oversight, and provider onboarding, all as part of our outsourcing medical billing services in US model.
We track each rejected or denied claim, fix errors or documentation gaps, then resubmit or appeal until resolution, ensuring no revenue gets lost.
You’ll receive monthly reports on clean claim ratio, first-pass success, denial rate, and AR metrics, transparent insight into our healthcare billing services performance.
Yes. Our team handles credentialing and payer enrollment nationwide, so you can join networks confidently without setup delays.
Most practices save up to 50% in admin costs and see collections increase by around 20-30% thanks to optimized HelloMD's medical billing and coding solutions.
We combine AAPC-certified coders, proprietary workflows, and full medical billing and coding solutions expertise. That means fewer errors, faster reimbursements, always.
Medical Billing What Is ERA in Medical Billing? Providers Guide…
ICD codes Global Period in Medical Billing: Rules, Codes &…