Guide to Medical Insurance Credentialing Process for Providers
Medical Insurance Full Process and Guide to Medical Insurance Credentialing…
Home / Understanding Modifier 33: Simplifying Preventive Services Billing
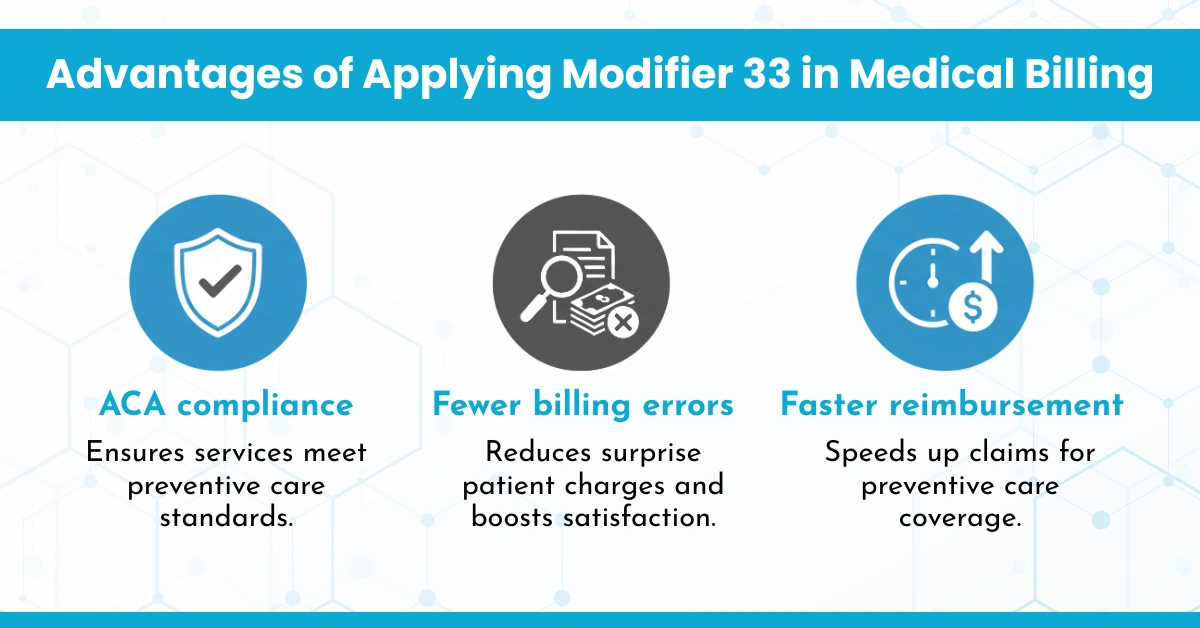
Accuracy in medical billing ensures that reimbursement and compliance occur without significant complications. Various distinctions found during the process include the utilization of it regarding the Affordable Care Act’s preventative services, enabling these to be billed under its guidance properly. In this blog, we will discuss Modifier 33 in detail.
Current Procedural Terminology, or CPT modifier 33, indicates a preventive service. It was added with the Affordable Care Act (ACA) in 2011. When billed properly, it ensures that patients can receive preventive services without spending out-of-pocket charges like copayments, deductibles, or coinsurance.
This modifier applies to services that meet the criteria for preventive care under the ACA guidelines. These include screenings, counseling, and preventive measures to detect or prevent illnesses before symptoms arise.
It should be added to CPT codes for services that are:
Modifier 33 is used for All Screenings: It applies only to services explicitly preventive under ACA guidelines. Diagnostic or follow-up services do not qualify.
Modifier 33 Eliminates All Patient Costs: While it signals a preventive service, some high-deductible plans may still require cost-sharing if services are outside ACA guidelines.
Modifier 33 is only for Primary Care Providers: Specialists performing preventive procedures (e.g., gastroenterologists performing colonoscopies) also use it when applicable.
Hello MDs streamlines the Modifier 33 process by automating the submission of preventive service claims, ensuring that the appropriate modifier is applied to eligible procedures. It indicates a preventive service exempt from cost-sharing under the Affordable Care Act, is automatically integrated into claims for qualifying services, reducing administrative burden for healthcare providers. This simplifies the billing process, ensuring compliance with regulatory requirements while improving reimbursement accuracy for preventive care services, ultimately enhancing efficiency and reducing coding and Medical billing errors.
Modifier 33 is an essential tool for aligning medical billing with the preventive care provisions required by the ACA. Proper use of this modifier ensures that patients receive necessary preventive services without additional costs and helps providers receive timely and correct reimbursement. By knowing the guidelines, healthcare providers can improve patient satisfaction and compliance while streamlining their billing processes.
Modifier 33 is a CPT code modifier used to indicate that the preventive services are those under the Affordable Care Act (ACA). The modifier ensures that patients are not charged for preventive services like screenings and immunizations. The service is, therefore, flagged to insurance companies as being preventive. This means that healthcare providers can ensure they have complied with ACA requirements, ensuring that patients are given preventive care without out-of-pocket costs.
It should be used when billing for services that are considered preventive under the ACA, including:
• Cancer screenings (e.g., mammograms, colonoscopies)
• Immunizations
• Preventive counseling (e.g., smoking cessation, weight loss)
• Other services recommended by the U.S. Preventive Services Task Force (USPSTF): For the service to indicate that it is preventive, it must be appended to the CPT code.
No, Modifier 33 only adds to those preventive services that qualify under the definition of the Affordable Care Act ACA’s preventive criteria. All tests are not qualifiers. A specific screening turns to diagnostic and should no longer be designated as preventive, e.g., a colonoscopy with which polyps get removed; similarly, certain prevention services might not even be reimbursed under plan policies. Further, payer policy defines the qualification under their coverage level.
While Modifier 33 guarantees that preventive services are covered under the ACA with no cost-sharing for eligible patients, some high-deductible health plans may still require patients to pay certain out-of-pocket costs. In addition, if a service is considered preventive but later becomes diagnostic, such as a biopsy taken during a screening procedure, the patient might be charged for the diagnostic portion.
Yes, improper use of Modifier 33 may cause claim denials or delayed payments. Ensuring that the service falls under the preventive category based on ACA criteria is essential. In the event of errors, audits, and penalties for uncorrected errors may be issued. Verify if the service is preventive and refer to payer-specific guidelines to avoid this mistake.
Medical Insurance Full Process and Guide to Medical Insurance Credentialing…
CPT Code CPT Code 99316 Description for Nursing Facility Billing…
ICD codes Medical Billing for Chiropractor: Complete Guide from HelloMDs…